Briefing / Summary of NHS operational planning and contracting guidance 2024/25
NHS England published a pack of operational planning and contracting guidance on 27 March 2024. Integrated care boards (ICBs) and their partner trusts must work with wider system partners and use this guidance to develop their system plans.
This briefing pulls out key points from all documents within the operational planning and contracting guidance pack, as relevant to NHS finance staff. It is not comprehensive and the full guidance should be referred to for greater detail.
Introduction
NHS England published a pack of operational planning and contracting guidance on 27 March 2024. Integrated care boards (ICBs) and their partner trusts must work with wider system partners and use this guidance to develop their system plans.
This briefing pulls out key points from all documents within the operational planning and contracting guidance pack, as relevant to NHS finance staff. It is not comprehensive and the full guidance should be referred to for greater detail.
It covers:
- Priorities and operational planning guidance
NHS England, Priorities and operational planning guidance 2024/25, March 2024
Document detailing national priorities for the NHS in 2024/25 and how ICBs and providers should incorporate these priorities into their plans - Revenue finance and contracting guidance
NHS England, Revenue finance and contracting guidance for 2024/25, March 2024
Guidance setting out financial expectations on NHS organisations - Elective Recovery Fund technical guidance
NHS England, Elective Recovery Fund technical guidance 2024/25, March 2024
Guidance on how the Elective Recovery Fund (ERF) will operate in 2024/25 - Capital guidance
NHS England, NHS capital guidance for 2024/25, March 2024
Document detailing NHS capital allocations for 2024/25
2024/25 priorities and operational planning guidance
The overall priority for the NHS in 2024/25 is to recover core services and productivity following the Covid-19 pandemic. The planning guidance acknowledges that this is a major challenge, which will take several years. In terms of the resources available, the spring Budget 2024 included £2.45bn of extra funding for the NHS in 2024/25, which is intended to cover the recurrent cost of the 2023/24 pay deal, with NHS funding otherwise being held flat.
As in 2023/24, finance is considered at a system level. ICBs, trusts and primary care providers are asked to work together to plan to deliver a net financial position which is balanced across the system. They should involve wider system partners as they decide how to balance various national and local priorities.
The focus on recovery is the same as in the previous year’s planning guidance. Within this, there is however now a sharper focus on productivity, and on how the NHS can be a better and more responsive employer.
Recovery
Nationally, the NHS continues to prioritise the recovery of core services – in particular, elective care, urgent and emergency care, NHS dentistry and access to primary care. The most significant financial mechanisms to support recovery are the same as those used in 2023/24. The Elective Recovery Fund (ERF) continues into 2024/25, and the Better Care Fund is being used to shift activity to settings outside acute hospitals.
To help recovery, systems are asked to maintain their bed numbers for general and acute care in 2024/25 at the same level funded and agreed through operating plans in 2023/24.
New in the 2024/25 planning guidance, NHS England is promoting NHS IMPACT,
Productivity
Previous planning guidance has prioritised productivity, but there is a sharper focus on it in 2024/25, with clearer expectations on systems.
NHS England expects all acute trusts to recover their productivity towards pre-pandemic levels (adjusted for structural factors, casemix changes and uncaptured activity). It asks ICBs to work with acute trusts to analyse their productivity compared to that in 2019/20 and put in place improvement plans. It also asks systems to review their workforce establishment against 2019/20, justify any increases (for instance based on outcomes, safety, quality or new service models) and put in place plans to improve workforce productivity.
Nationally, NHS England will start reporting on productivity metrics in the second half of 2024/25. This will go down to an ICB and trust level to enable systems to benchmark their performance. The core metrics will include:
- measures of overall productivity at trust level
- measures of operational and clinical productivity (such as the no criteria to reside rate, capped theatre utilisation, the diagnostic utilisation rate and turnaround time)
- measures of workforce productivity (such as outpatient appointments per consultant, care hours per patient day, bank and agency spend as a proportion of pay costs)
- measures of efficiency (such as on delivery of the opportunity for medicines optimisation).
As in previous years, the planning guidance includes a target on temporary staffing, though this year it has been elevated such that it’s included as one of the national objectives. NHS England asks systems to reduce their agency spend to a maximum of 3.2% of the total pay bill across 2024/25 (compared to a target of 3.7% in 2023/24). It also expects trusts to end their use of off-framework agencies by July 2024, and stipulates that any use of off-framework agencies before this point should be signed off by the chief executive or a designated deputy.
Supporting the NHS workforce
In 2024/25, the planning guidance has a much stronger focus on workforce than in previous years. It stresses the importance of improving staff experience, retention and attendance, saying ‘the evidence is clear that improving staff engagement will help to improve patient outcomes and safety’.
This is an area which is still under development, with more policies and guidance likely to follow within the next 12 months and in the coming years. The planning guidance sets out some specific requirements, but describes these as ‘the floor, rather than the ceiling, of our collective ambition to be a better and more responsive employer’.
Specific requirements are that NHS employers:
- implement the new National pregnancy and baby loss people policy framework
NHS England, National pregnancy and baby loss people policy framework, March 2024 - implement the NHS sexual safety charter
NHS England, Sexual safety in healthcare – organisational charter, September 2023 - implement the actions and best practice available through the retention hub
NHS England, Looking after our people – retention hub - embed the NHS equality, diversity and inclusion improvement plan
NHS England, NHS equality, diversity and inclusion (EDI) improvement plan, June 2023 - align their training with the Core skills training framework
Health Education England, Core skills training framework (England), June 2021 - implement the Growing occupational health and wellbeing together strategy
NHS England, Growing occupational health and wellbeing together strategy - provide work schedules in advance, with compassionate on-call rostering and leave request management.
Detailed priorities, targets and actions
Beyond the key themes of recovery, productivity and supporting the workforce, the planning guidance explains the actions that systems should take to support a more detailed set of national objectives.
Table 1 lists the national objectives and explains where they are different to those used in 2023/24. The page numbers refer to the Priorities and operational planning guidance 2024/25,
There are two segments which instruct systems on the actions they should take, but which do not tie directly back to any of the national objectives listed in table 1. These are on digital and data (page 30) and system working (page 34).
In terms of finance, a segment on use of resources (page 31) explains where NHS England expects systems to find the greatest efficiency savings. It calls on systems to:
- reduce unwarranted variation in the cost of continuing healthcare placements
- optimise medicine value (by reviewing prescribing trend data each month, increasing the use of generics and biosimilars, and delivering against the national medicines optimisation opportunities)
- reduce the cost of running corporate services
- procure energy through a new national contract developed with Crown Commercial Services
- use the consolidated supplier frameworks agreed through NHS Supply Chain and procure from frameworks operated by an accredited framework host.
Some of the national objectives from 2023/24 are no longer included in the 2024/25 guidance. For example, there are no longer objectives on bed occupancy, the number of general practice appointments, or the Additional Roles Reimbursement Scheme (ARRS) for primary care.
Table 1: Comparing the 2024/25 national objectives to 2023/24
| Area | Objective (and page reference to planning guidance) | Changes since 2023/24 |
|---|---|---|
| Quality and patient safety | Implement the Patient Safety Incident Response Framework (PSIRF) (Page 12) | 🆕 |
| Urgent and emergency care | Improve A&E waiting times, compared to 2023/24, with a minimum of 78% of patients seen within 4 hours in March 2025 (Page 13) | Increase from 76% target in 2023/24. |
| Improve Category 2 ambulance response times to an average of 30 minutes across 2024/25 (Page 13) | Timeframe pushed back by 12 months. Otherwise no change. | |
| Primary and community services | Improve community services waiting times, with a focus on reducing long waits (Page 17) | 🆕 |
| Continue to improve the experience of access to primary care, including by supporting general practice to ensure that everyone who needs an appointment with their GP practice gets one within 2 weeks and those who contact their practice urgently are assessed the same or next day according to clinical need (Page 16) | - | |
| Increase dental activity by implementing the plan to recover and reform NHS dentistry, improving units of dental activity (UDAs) towards pre-pandemic levels (Page 17) | New reference to plan to recover and reform dentistry. Otherwise no change. | |
| Elective care | Eliminate waits of over 65 weeks for elective care as soon as possible and by September 2024 at the latest (except where patients choose to wait longer or in specific specialties) (Page 18) | Timeframe pushed back by 6 months. Otherwise no change. |
| Deliver (or exceed) the system specific activity targets, consistent with the national weighted activity target of 107% (Page 19) | - | |
| Increase the proportion of all outpatient attendances that are for first appointments or follow-up appointments attracting a procedure tariff to 46% across 2024/25 (Page 18) | 🆕 | |
| Improve patients’ experience of choice at point of referral (Page19) | 🆕 | |
| Cancer | Improve performance against the headline 62-day standard to 70% by March 2025 (Page 19) | Introduction of percentage target. |
| Improve performance against the 28 day Faster Diagnosis Standard to 77% by March 2025 towards the 80% ambition of 95% (Page 19) | Increase from 75% target in 2023/24. | |
| Increase the percentage of cancers diagnosed at stages 1 and 2 in line with the 75% early diagnosis ambition by 2028 (Page 20) | - | |
| Diagnostics | Increase the percentage of patients that receive a diagnostic test within six weeks in line with the March 2025 ambition of 95% (Page 21) | - |
| Maternity, neonatal and women's health | Continue to implement the three-year delivery plan for maternity and neonatal services, including making progress towards the national safety ambition and increasing fill rates against funded establishment (Page 22) | New reference to three-year delivery plan. Otherwise no change. |
| Establish and develop at least one women’s health hub in every ICB by December 2024, working in partnership with local authorities (Page 23) | 🆕 | |
| Mental health | Improve patient flow and work towards eliminating inappropriate out of area placements (Page 23) | New reference to patient flow. Otherwise no change. |
| Increase the number of people accessing transformed models of adult community mental health (to 400,000), perinatal mental health (to 66,000) and children and young people services (345,000 additional CYP aged 0-25 compared to 2019) (Page 23) | Introduction of target numbers for adult community and perinatal mental health. No change on CYP. | |
| Increase the number of adults and older adults completing a course of treatment for anxiety and depression via NHS Talking Therapies to 700,000, with at least 67% achieving reliable improvement and 48% reliable recovery (Page 23) | Introduction of specific targets on number and percentages. | |
| Reduce inequalities by working towards 75% of people with severe mental illness receiving a full annual physical health check, with at least 60% receiving one by March 2025 (N/A) | 🆕 | |
| Improve quality of live, effectiveness of treatment, and care for people with dementia by increasing the dementia diagnosis rate to 66.7% by March 2025 (Page 23) | - | |
| People with a learning disability and autistic people | Ensure 75% of people aged 14 and over on GP learning disability registers receive an annual health check in the year to 31 March 2025 (Page 25) | - |
| Reduce reliance on mental health inpatient care for people with a learning disability and autistic people, to the target of no more than 30 adults or 12-15 under 18s for every 1 million population (Page 25) | - | |
| Prevention and health inequalities | Increase the percentage of patients with hypertension treated according to NICE guidance to 80% by March 2025 (N/A) | Increase from 77% target in 2023/24. |
| Increase the percentage of patients aged 25-84 years with a cardiovascular disease (CVD) risk score greater than 20% on lipid lowering therapies to 65% by March 2025 (N/A) | Increase from 60% target in 2023/24. | |
| Increase vaccination uptake for children and young people year on year towards WHO recommended levels (Page 26) | 🆕 | |
| Continue to address health inequalities and deliver on the Core20PLUS5 approach, for adults and children and young people (Page 27) | - | |
| Workforce | Improve the working lives of all staff and increase staff retention and attendance through systematic implementation of all elements of the People Promise retention interventions (Page 28) | New reference to the working lives of all staff. Otherwise no change. |
| Improve the working lives of doctors in training by increasing choice and flexibility in rotas, and reducing duplicative inductions and payroll errors (N/A) | 🆕 | |
| Provide sufficient clinical placements and apprenticeship pathways to meet the requirements of the NHS long term workforce plan (Page 29) | - | |
| Use of resources | Deliver a balanced net system financial position for 2024/25 (Page 31) | - |
| Reduce agency spending across the NHS, to a maximum of 3.2% of the total pay bill across 2024/25 (Page 31) | 🆕 |
Revenue finance and contracting guidance
The business rules in the NHS financial framework
Each system will need to map the financial position of their ICB and trusts into their system plans. Separately, trusts are also asked to submit organisational financial plans to NHS England, and it is important that these match up to the plans submitted at a system level.
2024/25 is the first year that some systems will be making repayments on overspends from previous years. After overspending, systems are given two years to recover their finances before having to make repayments. Any system which overspent in 2022/23 will therefore start making repayments in 2024/25.
NHS England stresses that it does not expect widespread access to drawdown in 2024/25, and that systems should not assume access to drawdown unless NHS England has approved this in advance of the plan submission.
Table 2: ICB and system finance business rules
| Rule | ICB | System |
|---|---|---|
| Capital resource use | Collective duty to act with a view to ensuring that the capital resource use limit set by NHS England is not exceeded | |
| Revenue resource use | Duty to meet the resource use requirement set by NHS England | Collective duty to act with a view to ensuring that the revenue resource use limit set by NHS England is not exceeded |
| Breakeven duties (achieve financial balance) | Duty to act with a view to ensuring its expenditure does not exceed the sums it receives | Objective to break even – that is, duty to seek to achieve system financial balance |
| Financial apportionment | Revenue and capital resources of all trusts apportioned exclusively to a principal ICB | |
| ICB administration costs | Duty not to exceed the ICB running cost allowance limit set by NHS England | |
| Risk management | Local contingency decision required to show how financial risks will be managed | |
| Prior year’s under and overspends | Maintain as a cumulative position | |
| Repayment of prior year’s overspends | All overspends are subject to repayment | |
| Mental Health Investment Standard | Comply with standard | |
| Better Care Fund | Comply with minimum contribution | |
ICB revenue allocations
NHS England has updated its ICB revenue allocations for 2024/25.
Some key changes are that:
- The net cost uplift factor has reduced to 0.6% (originally expected to be 0.7%). This is made up of an estimated 1.7% inflation, netted off by a 1.1% general efficiency requirement (originally expected at 1.8% and 1.1%). Full details on the assumptions behind this calculation are set out in Annex D of the 2023/25 NHS payment scheme.
NHS England, 23-25 NHS payment scheme - amended Annex D Prices and cost adjustments, March 2024 (see section 4 on ‘setting cost uplift and efficiency factors for 2024/25’) - Baseline adjustments have been made to include pay funding issued in 2023/24 on a recurrent basis, non-pay inflation as confirmed during 2023/24, and funding to cover the revenue impact of IFRS 16.
- Funding announced since the 2024/25 allocations were first released has been added in. This includes funding for ambulance services, urgent and emergency care capacity, and continued Covid-19 testing.
- Base growth has increased by 1.0% to reflect pressures since the original 2024/25 allocations were published, factoring in a revised growth domestic product (GDP) deflator.
- ICBs over their target allocation will move more slowly towards target, with convergence values scaled back to 80% of what was in the original allocations. The convergence value has not changed for ICBs that are under their target allocation.
ICB running cost allowance
NHS England has previously announced that ICBs must reduce their running cost allowance by 30% in real terms by 2025/26, with at least 20% to be delivered in 2024/25.
Service Development Fund (SDF) and Elective Recovery Fund (ERF)
SDF and ERF will both continue into 2024/25 in much the same format as in 2023/24. NHS England has streamlined the number of individual allocations it makes by bundling SDF categories together into high-level groupings. Several categories (including for mental health) are still ringfenced, with funding to be returned if it is underspent. Further details are available from NHS England, and each ICB should receive a separate schedule and technical guidance. On the ERF, NHS England has produced additional guidance, which is summarised on page 11 of this document.
Delegation in 2024/25
Selected acute specialised services are being delegated to ICBs in the East of England, Midlands and North West regions from 1 April 2024. ICBs in other regions will work with NHS England through statutory joint commissioning arrangements, whereby regional commissioners submit their specialised commissioning plans at an ICB level, with approval from the relevant ICBs. (Statutory joint commissioning will also be used for specialised services which are out of scope for delegation in the East of England, Midlands and North West regions.)
NHS England introduced a new allocations methodology for specialised services in 2023/24 and has made further updates in 2024/25. A needs-based formula replaces the previous formula which was based on consumption of services, and convergence requirements mean that funding in some areas will be reduced such that ICBs move towards their fair share.
Arrangements for specialised high-cost drugs and high-cost devices will stay the same as in 2023/24 (even for ICBs where specialised commissioning has been delegated). Allocations will stay with NHS England, and NHS England will manage the reimbursement to trusts.
Future delegation
The revenue finance and contracting guidance refers to a number of services which will be commissioned by NHS England through 2024/25, but may be delegated in the future. These are:
- Specialised mental health, learning disability and autism services
Phase 1 NHS-led provider collaboratives have now been set up. NHS England’s regional commissioning teams currently contract these services with lead providers, and they may be delegated to ICBs in 2025/26. - Public health services
NHS England’s regional commissioning teams currently contract services that form part of the NHS public health functions (Section 7A) agreement. To help prepare for future delegation, the regional teams will produce 2024/25 financial plans for public health services at an ICB level.
Revenue support for capital
The government recently agreed additional revenue resources to support the NHS with depreciation and amortisation expenditure. Owned assets and leased right-of-use assets may be in scope for additional funding if, at a system level, the depreciation and amortisation on these assets exceeds a level set by NHS England. To claim this funding, systems will need to come together to plan their depreciation and amortisation expenditure.
As in previous years, New Hospital Programme (NHP) schemes are eligible for relief on public dividend capital (PDC) on their assets under construction, such that trusts will not pay PDC before the asset is operational. This is now being extended to a small number of schemes outside the NHP.
As in 2023/24, ICBs have been given dedicated revenue funding to contribute to the set up and running costs of community diagnostic centres. Further guidance will follow, but to pay trusts for this work, ICBs will need to submit a request to NHS England for a locally-agreed adjustment to the aligned payment and incentive (API) rules.
NHS payment scheme
A new version of the NHS payment scheme came into effect on 1 April 2024.
The NHS payment scheme applies to all secondary healthcare and give rules for four payment mechanisms: aligned payment and incentive (API), low volume activity (LVA), activity-based payments, and local payment arrangements.
Most healthcare provided by trusts will come under an API agreement, which includes both a fixed element and a variable element for elective activity. Appendix 1 of the Revenue finance and contracting guidance gives advice on how to calculate the fixed and variable elements.
As before, LVA arrangements will apply to most trust-ICB relationships with an expected annual value below £0.5m. To simplify the mechanism for delegated services, in 2024/25, ICBs should add the LVA value of delegated services onto existing LVA contracts so that a single payment can be made for all services. There will be a small number of exceptions to this, where NHS England considers delegated services to be of significant value and therefore better managed under API.
NHS England has decided to pause its nationally-mandated commissioning for quality and innovation (CQUIN) incentive scheme in 2024/25. Fixed payments should include the 1.25% funding previously identified for CQUIN as guaranteed income for providers.
Financial commitments and key assumptions
The revenue finance and contracting guidance sets out a number of financial commitments and key assumptions that it expects systems to make as part of their planning process. These are set out in Table 3.
Table 3: Financial commitments and assumptions for planning
| Area (and page number to revenue and contracting guidance) | Financial commitment or assumption |
|---|---|
| Mental health (page 31) | ICBs must increase spending on mental health services in line with the mental health investment standard (MHIS). Any efficiencies from MHIS-related expenditure should be reinvested in mental health services such that systems continue to meet their MHIS requirements. This is a commitment from the NHS long term plan. |
| Better Care Fund (page 31) | ICBs must pool allocations for the Better Care Fund into Section 75 agreements alongside grants paid to local government. This is a commitment from the autumn Statement 2022. |
| Agency staff (page 32) | Systems must reduce their agency spend. Systems have been set different targets based on their current performance, with an aim that agency spending for all trusts will be no more than 3.2% of the total NHS pay bill. This is a commitment from the spring Budget 2024. |
| Dental ringfence (page 33) | ICBs must ensure that the dental budget in the pharmaceutical, ophthalmic and dental (POD) allocation is ringfenced to dental care. This is to support the dental recovery plan. |
| Charge-exempt overseas visitors and UK cross-border emergency activity (page 34) | ICBs should expect minimal in-year changes to core programme allocations in respect of charge-exempt overseas visitors and UK cross-border emergency activity. (These allocations can be redistributed in-year based on activity, but are currently based on 2023/24 figures.) |
| Clinical negligence scheme for trusts (CNST) (page 35) | Commissioners must uplift the fixed element of their contracts for maternity using the maternity CNST uplift. They must also apply a CNST uplift to other service areas, but can use an average figure for non-maternity if it is too resource intensive to apply the uplift at a service level. |
| Covid-19 testing (page 36) | ICBs and trusts should assume that the Covid-19 testing protocol published in March 2023 will remain in place through 2024/25. ICB plans should not include any income or expenditure relating to testing through the community pharmacy advanced service. |
| Inflation (page 36) | The net cost uplift factor for 2024/25 is 0.6%. This is made up of 1.7% inflationary pressures, off-set by a 1.1% efficiency requirement. Within the inflationary pressures, NHS England expects a 2.1% increase to pay costs, a 0.3% increase to drugs, 0.8% to capital, 0.6% to unallocated CNST and 0.8% to other costs. |
| Consultant pay (page 36) | Trusts should hold in reserve (and not spend) and funding relating to Local Clinical Excellence Awards (LCEAs). The consultant pay reform offer (which is still being voted on) includes a proposal to redeploy funding from the LCEAs to main pay. At this stage, there has been no cost uplift to reflect the offer, but as and when a pay uplift is agreed, NHS England is assuming that the LCEA funding will cover the first 1.5 percentage points. |
| NHS pensions (page 37) | NHS employers should not factor in any changes to the employer contribution rate on the NHS pension scheme. Transitional arrangements continue, and employers will continue to pay a contribution rate of 14.38% in 2024/25. |
| Central technology licensing arrangement (page 37) | ICBs should reflect in each trust’s API fixed payment value the transfer of ICB allocations for trust technology licences. |
| Non-NHS commissioners (page 38) | Trusts should ensure that contracts with non-NHS commissioners (such as local authorities) include inflationary uplifts for 2023/24 and 2024/25 pay. |
| Drawdowns (page 6) | Systems should not assume access to drawdown unless NHS England has approved this in advance of the plan submission. |
| Primary care (page 10) | ICBs should assume that the full increase in allocations for primary care is needed to fund growth and contractual payment increases. The government is yet to respond to the 2023/24 Review Body on Doctors’ and Dentists’ Remuneration. |
| Community pharmacy services (page 11) | ICBs should not include income or expenditure for Pharmacy First in their plans. Further guidance on payment terms and pass-through funding arrangements will follow. |
| Covid-19 vaccination services (page 21) | Systems and trusts should not include income or expenditure for Covid-19 vaccination services in their plans. The government has not yet approved funding for Covid-19 vaccination services. |
| Education and training funding (page 21) | Systems will be given a set of assumptions for use until the 2024/25 education and training tariff is published |
Elective Recovery Fund technical guidance
NHS England is running the Elective Recovery Fund (ERF) in much the same way as in 2023/24, to make it as easy as possible to understand and apply in 2024/25.
There is £3.2bn of funding for ERF in 2024/25 (compared to £3.1bn in 2023/24). Nationally, the NHS is expected to use this to deliver 107% of the activity delivered in 2019/20 – the same level as in 2023/24 before NHS England adjusted for industrial action. Each commissioner will be set the same target as at the start of 2023/24.
The ERF will have the same funding flows between NHS England and ICBs. NHS England will hold back 18% of each ICB’s ERF allocation and release it when the ICB reaches the required levels of elective activity. It will also provide additional funding for any ICB that exceeds its overall target.
Providers will continue to be paid for the elective activity they deliver. Commissioners will pay providers at 100% of the prices in the 2023/25 NHS payment scheme,
Changes to baseline
There are minimal changes to baselines. The baselines take 2019/20 value-weighted activity (as agreed for 2023/24) and adjust for the profile of working days in 2024/25. The activity is then valued using 2024/25 NHS payment scheme unit prices.
For simplicity, low value activity relationships
Changes to targets
There are minimal changes to targets. At a national and a commissioner level, the targets in 2024/25 are the same as at the start of 2023/24 (before later adjustments for industrial action).
NHS England will publish a detailed set of activity baselines and targets, which will break down what each individual provider is expected to deliver with each individual commissioner. Commissioners and providers can negotiate alternative targets, but the NHS England figures will be used as a default if they cannot agree.
One change in 2024/25 is that NHS England’s detailed, provider-level targets now reconcile fully to the overall commissioner targets. Any commissioner which agrees different targets with its providers must make sure that these agreements still add back to their overall commissioner target.
Changes for specialised commissioning
The most significant changes relate to specialised commissioning, as NHS England is delegating more of its specialised commissioning to ICBs in 2024/25.
NHS England is aiming to maintain the position for providers as much as possible, though different commissioners will be involved. In 2023/24, NHS England had one ERF agreement for specialised services with each relevant provider. In 2024/25, it is saying that for specialised services, each provider will have only one commissioner dealing with the variable ERF payments.
Where specialised services have been delegated to an ICB, the ICB will make ERF agreements with all providers within its system for all the specialised services it delivers (including to patients from other ICBs). Where specialised services have not been delegated, NHS England make ERF agreements with providers as before. NHS England will also pay all specialist top-ups, even where specialised services are delegated. No ICB should make an ERF agreement with a provider outside of its system. Further details are included at Appendix 3 to the guidance (page 15).
Capital guidance update
The NHS capital guidance 2022 to 2025 still applies,
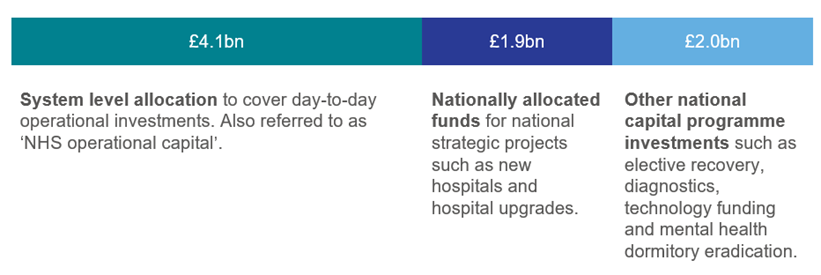
The total allocation across England is £8bn, as shown in Figure 1. As in previous years, this is split into three categories: a system level allocation, national allocated funds and other national capital programme investments. This allocation excludes IFRS 16 adjustments, which will be added later in the planning process.
Figure 1: Capital allocations
System level allocation
The baseline allocations for ICBs’ operational capital have not changed since they were first set out in the 2022 to 2025 capital guidance. This makes up over 90% of the system level allocation.
Around 7% of the system level allocation will be distributed according to incentive schemes that have been announced and communicated to ICBs and providers previously:
- Finance incentive
£150m incentive, to be shared among qualifying ICBs. ICBs qualify for a share if their system delivers a surplus, and a partial share if their system delivers on a deficit plan that has been agreed by NHS England. - Urgent and emergency care incentives
£150m incentive, to be shared among qualifying providers. Providers qualify for a share if they have a Type 1 A&E department, achieved 80% A&E four-hour performance from January to March 2024, and completed at least 90% of ambulance handovers within 30 minutes from October 2023 to March 2024. Providers will also be eligible for further funding up to £4m based on their A&E four-hour performance in March 2024.
Systems should factor the finance incentive into their capital plans based on their expected revenue outturn in 2023/24. They should not however factor in any payments for the urgent and emergency care incentives. NHS England will confirm these allocations at a later stage once the performance data is available.
The final part of the system level allocation goes on a small number of national operational capital programmes – for ambulance replacements, maternity neonatal cots and aseptic monitors. NHS England will apply uplifts to any payments which are due for these in 2024/25.
For the 2024/25 planning, NHS England will accept systems or regions over-programming by up to 5% of their operational capital allocation, so long as there is a clear plan that allows elements to be scaled back if necessary.
Nationally allocated funds
The guidance does not signal any changes to the national capital programmes, targets, draw-down procedures or reporting requirements. One change is that the national estates team is working on a national capital reporting tool, which will help project teams to profile, forecast and report their spend. Once it is available, all estates schemes that are part of a national programme delivered through public dividend capital (PDC) will be asked to use this platform.
Other national capital programme investments
The guidance focuses on diagnostics and technology transformation, but does not indicate any changes in targets or policy direction. Less funding is available in 2024/25 for integrated care systems to meet minimum digital foundations (a minimum of £400m compared to a minimum of £500m in 2023/24). This is for systems to develop their electronic patient records and scale up their use of digital social care records.
Treatment of IFRS16: Leases
Nationally, there is an £800m CDEL uplift to cover the impact of IFRS16 in 2024/25, which is in addition to the £8bn capital allocation outlined above. However, this will be added to system budgets later in the process. At plan stage, no IFRS 16 uplifts will be made to system operational capital allocations.
Systems and providers are asked to complete their planning returns on an IFRS16 compliant basis, using an IFRS16 uplift no more than 30% higher than in 2023/24. The design of the forms is such that the IFRS16 elements can easily be included or excluded for review.
After the planning process, NHS England will add the IFRS16 uplifts to the operational capital allocations, and systems will need to manage their capital spend against their total operational capital allocation, including the impact of IFRS. Any overspends will be deducted from the 2025/26 capital allocations.
Other requirements
Beyond the ordinary course of reporting, the latest guidance explains specific circumstances when ICBs or providers should notify NHS England. These are set out below.
- If a system is unable to deliver by the end of March 2025 on the ambulance replacement, maternity neonatal cots or aseptic medicines programmes. (Notify NHS England capital and cash team as soon as possible.)
- If a system is planning a land and property disposal and intends to treat this as a CDEL credit over multiple years. (Notify NHS England by the month 6 submission at the latest.)
- If a provider recognises there is a risk of a PFI or LIFT project terminating due to default of the project co party. (Notify NHS England as soon as possible.)
- If a provider or ICB is anticipating a significant new lease and lease amendments within the scope of IFRS in 2024/25. (Discuss with NHS England regional finance teams as soon as possible.)
Related content
The HFMA mental health conference is a learning and development event and is the largest face to face event for the HFMA Hub mental health network.
The Engagement Value Outcome (EVO) Framework has been designed to help teams improve patient care at the system level
