System efficiency:working together
New models of integrated care can only be delivered by whole systems. Similarly delivering services within current budgets and maintaining the sustainability of those services demands a system approach – otherwise a saving in one organisation could lead to higher costs elsewhere. Pressure to work as systems is increasing and one sustainability and transformation partnership (STP) has started to think about practical ways to take a broader view to the efficiency challenge.
‘We simply haven’t met in the past to look at efficiency collectively,’ says Suzanne Robinson (pictured below), director of finance, performance and digital at North Staffordshire Combined Healthcare NHS Trust and recently appointed Together we’re better finance director of Staffordshire and Stoke-on-Trent’s Sustainability and Transformation Partnership.
‘Traditionally there has been a challenge with the development of efficiency plans – whether they are commissioners’ quality innovation productivity and prevention (QIPP) plans or providers’ cost improvement programmes (CIPs) – which are often pulling in different directions. So what we’re trying to do is to strengthen the links between clinical commissioning groups, providers, NHS England and NHS Improvement and move to co-production or joint ownership of these plans.’
From this month, this will see a new STP efficiency group established to take a more rounded view of the productivity challenge facing all organisations in the health economy individually and collectively. Chaired by Ms Robinson, the group will involve deputy finance directors and senior finance managers, and report back to the STP’s overarching finance director forum.
‘There has been a tendency for us all to look at what we can do individually in our organisations, and we’re often very successful at that,’ says Ms Robinson. However, this approach can sometimes lead to unintended consequences. So a saving in one organisation can lead to a cost pressure within another. ‘What we’re looking for is an approach where we are working collaboratively to incentivise transformation and, where there is a saving for the system as a whole, we don’t overlook this based on the impact on individual organisations.’
However, the scale of the current challenge means that tackling efficiency in silos is no longer an option. ‘We’ve been discussing within our leadership forums ways in which we can mitigate those financial pressures that individual organisations face, where it’s clear there is a bigger benefit for the system and for the longer term sustainability of our economy,’ says Ms Robinson. ‘We’re clear that this group shouldn’t replace the work within existing organisations, particularly the importance of transformation schemes being clinically led; but there is a role for finance professionals and we do have a valuable contribution.’
There are clear tensions between a regulatory system that remains focused on individual organisational performance and calls to operate as whole health economies. But system working is the clear focus.
STPs’ role
February’s refreshed planning guidance for 2018/19 made it clear STPs should take ‘an increasingly prominent role in planning and managing system-wide efforts to improve services’. This should involve ensuring key, credible assumptions on finance and activity are used in both provider and commissioner plans. Where these assumptions do not enable all the concerned organisations to meet their control totals, ‘the STP will need to agree additional cost containment measures and highlight any implications’.
STPs were also told to lead efforts to ‘identify system-wide efficiency opportunities such as reducing avoidable demand and unwarranted variation, or sharing clinical support and back office functions’.
The future direction of travel is also clear. The existing 10 integrated care systems (the eight original shadow accountable care systems and the two devolved health and care systems) have been told to focus on delivery of system control totals (currently a simple sum of organisation control totals). For 2018/19, these systems will only receive their share of the additional £650m put into the newly named provider sustainability fund (PSF) if the system control total is met. But from 2019/20, a full system-based approach will see their payments from the whole PSF and the parallel commissioner sustainability fund (CSF) tied to achievement of the system control total.
So it is clear organisations will have to take a much bigger interest in the ability of all parts of a system to deliver efficiencies that enable them to deliver against individual and system control totals. It is something local leaders in Staffordshire and Stoke-on-Trent are bought into.
‘The traditional win-lose approaches to efficiency – run faster, do more with the same/less – have proved to be unsustainable and unproductive, especially within systems where resource is diminishing relative to the demand coming through the system,’ says Alistair Mulvey (pictured), chief finance officer of the six Staffordshire and Stoke-on-Trent CCGs. ‘Increasingly there is an awareness that marginal gains, while needing to be maintained, must be supplemented with material pathway and service delivery change. Without these stepped changes, then the resource utilisation will continue to be imbalanced.’
He believes that if a systems-wide approach is not adopted – with clinically led change programmes – the future will be about the ‘management of decline’, which would be neither sustainable nor in patients’ interests. ‘The answer lies in systems-based, authentic, open and honest engagement around efficiency improvements and management of these changes with the focus on patients being paramount,’ he says.
Staffordshire challenge
Staffordshire and Stoke-on-Trent’s challenge is arguably bigger than most. It was one of just a handful of STPs identified as ‘needing most improvement’ in last summer’s baseline STP progress dashboard. It was also one of the 14 STPs put into the capped expenditure process. And some of its five providers are running significant deficits.
The STP’s sustainability and transformation plan predicted a gap of £286m in health funding by 2020/21 if no changes were made to current care models and demand continued to rise. This increased to £542m when social care was factored in. Continuing pressures across the healthcare sector have done little to suggest that the forecast gap is closing.
To address this, the STP has been looking at a number of workstreams including: focused prevention; enhanced primary and community care; effective and efficient planned care; simplified urgent and emergency care; mental health; and maternity and children. It is looking at these issues with two distinct timeframes in mind: over one to five years (affordable care) and over three to 10 years (transforming care).
The sustainability and transformation plan acknowledges that the economy has been living beyond its financial means for a number of years, yet it continues to exhibit health inequalities across the system (between Stoke-on-Trent and parts of Staffordshire for example) and underperforms when compared with other areas on some key outcomes.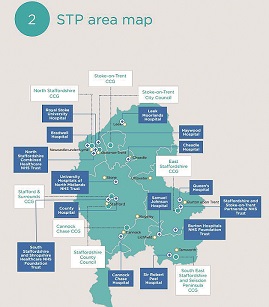
It has high levels of avoidable admissions, high cost of urgent and emergency care, duplication of planned care services and too much estate. STP director Simon Whitehouse says that quality of care is the driving force. ‘We’ve not got the luxury of funding any double running,’ he says – the health economy can’t invest in community and general practice while at the same time funding acute services to keep meeting the current levels of demand.
It has to find ways to change the model of care within the existing financial envelope. ‘We are currently spending more than we should and we are not delivering the outcomes we want or turning back the dials on health inequalities in the right direction across the board. We need to do better for the local population that we serve, but also have to recognise that housing, education and employment opportunities have a much bigger impact on some of these areas. So we have to work on those aspects as well with our partners,’ he says. Even if there was additional funding available, the health economy would still need to change its service model.
All service changes are being clinically led and a new community model involving multidisciplinary teams working in 23 localities within three geographical alliance footprints is central to transformation plans.
The new efficiency group aims to support this broader work, challenging the workstreams on efficiency opportunities by providing detailed examples of where the STP is a financial outlier, where variation is unwarranted or where opportunity exists.
Mr Whitehouse believes that dealing with any duplication and variation ‘in a way that makes most sense for our clinicians and for our patients is essential’. ‘There is a valid challenge from the public – before you start talking to us about cutting services and reducing clinical staff, can you tell me that you’ve done everything you can to ensure you are as efficient as possible,’ he says. ‘We need to be able to say we’ve gone as far as we can with utilities, estates, staff and rotas and use of agency.’ And he adds that this means exploring whether greater efficiency can be achieved working as systems rather than in isolation.
‘Organisations have been hardwired to look after themselves and it is no surprise that they’ve done this very well,’ he says. ‘But does every organisation need its own payroll or can we get a better deal if we are all on the same payroll?’ He stresses that bigger isn’t always better, but the options need to at least be explored and the current arrangements challenged.
Getting the organisations in the system to work through these issues, rather than imposing decisions from the STP, is seen as the best way to ensure different stakeholders own the decisions.
A set of principles to support the co-production of efficiency plans has already been drafted by the STP organisations with a view to adopting these into contracts. The overarching aim is to focus on getting ‘value from the overall health pound’, says Ms Robinson.
Mr Mulvey says that systems can help meet patient demand in better ways. ‘For example, with nursing homes, we find that the number of patients admitted into acute settings continues to cause pressure,’ says Mr Mulvey. But this demand curve can be bent downwards by working with primary care to ensure a single GP looks after a cohort of patients in a home (rather than multiple GPs with several patients each). This can then be supported with greater access to community services such as IV antibiotics or advice lines and support from pharmacy technicians.
‘This can lead to patients increasingly being cared for in their nursing homes rather than conveyed to hospital multiple times,’ Mr Mulvey adds. The outcome is better for the patients and delivers better overall value. The scheme is currently being piloted in 28 homes across the north of the county with early results demonstrating a 15% reduction in A&E attendances from the homes involved.
Other organisations in the STP agree with a collective approach. University Hospitals of North Midlands NHS Trust was placed into financial special measures a year ago. Chief finance and performance officer Helen Ashley says that since then the trust has focused on its own internal efficiencies. ‘But given the scale of the financial challenge that the trust and commissioners face, it’s clear that by working with colleagues across the economy there are far more opportunities to generate efficiencies – something that we have not historically focused on,’ she says. ‘At the end of the day there is only one pot of money and, therefore, we all have a duty to work collectively to ensure best use is made of the limited resource that we have.’
This approach to efficiency should also help sidestep some of the existing barriers to improvement. ‘For example, in very simple terms, consider if we wanted to change a service and it means the commissioner pays £1m less to a provider,’ says Ms Robinson.
‘If that provider can only release the £0.5m of variable costs and is left with £0.5m fixed costs, on the basis that the system is £0.5m better off overall, we can agree a mechanism to cover these costs for a period of time. We are looking to remove those disincentives [for the provider] and to allow for transformation to take place and costs to be removed.’
Wider engagement
The sub-director level involvement in the group is important. ‘We are deliberately trying to cast the net further and engage more of the finance community,’ Ms Robinson explains. ‘Sometimes the STP is visible at the very senior level in organisations, but as you drop down, there is less involvement. We’re keen for all our staff (and specifically in finance) to see the STP as a collective whole, not a few individuals. We want everyone to be aware of what the STP is about and for everybody’s day-to-day work to be about delivering this plan.’
The group will use NHS England’s 10-point efficiency plan as the focus for its discussions. There are already issues that the group wants to explore – such as how different bodies contract for different IM&T services. ‘There may well be an opportunity to rationalise those arrangements across the system,’ says Ms Robinson.
With the engagement CQUIN now worth 1% of contract value, as a result of the refreshed planning guidance, the group will also explore ways in which specific criteria could be used to trigger payment and encourage further joint working. And it is aiming to develop a better understanding of what efficiency schemes are actually delivering, with the intention of ruling out double-counting of organisational efficiencies as improvements secured by the STP.
Another area the group will look at involves contract breaches. ‘In the system we have created, it is very easy to send letters to each other when you breach contractual targets or data requirements,’ she says. ‘But does this always add value and would we be better using the time and energy to agree an outcome or an efficiency scheme and then work collectively to achieve that? We are just looking for better ways to work together.’ She adds that the group may also examine the potential to combine forces and purchase things together where that makes sense – for example, IT service contracts or corporate services procurement.
Both NHS Improvement and NHS England will be represented on the group and Ms Robinson says the involvement of both regulators has already started to add value to their discussions.
The group’s terms of reference state it will develop ‘creative and forward thinking ideas that push the boundaries of possibilities with the aim of making the STP a leading light in terms of innovation, progress and delivery’. It will also lead the health economy’s thinking on moves to different payment systems – such as population health budgets – to better incentivise and support new models of care.
There are some significant challenges in Staffordshire and Stoke-on-Trent. But all health economies are facing similar issues. All health economies need to understand what efficiencies can be realised at the system level and many may see Staffordshire and Stoke-on-Trent’s efficiency group as a possible vehicle to help explore this area.
Convergence 2.0
Last year’s Convergence event brought together the HFMA’s annual commissioning and provider conferences to focus on moves towards accountable care. A year later, the terminology has changed, with ‘integrated care’ being the new preferred description. But the agenda is still very much about finding the best ways for organisations to work together to deliver services that meet the needs of individuals and populations. This involves establishing new models of care, supported by new governance arrangements and underpinned by new payment systems that are aligned with overarching system goals. Convergence 2.0 will provide practitioners with an update on progress across the country, as well as drilling down into the detail of some of the areas making the most progress with integration.
For more details on Convergence 2.0, click here
Related content
The Institute’s annual costing conference provides the NHS with the latest developments and guidance in NHS costing.
The value masterclass shares examples of organisations and systems that have pursued a value-driven approach and the results they have achieved.