News / Providers end year with £2.45bn deficit
 Publishing the figures, NHS Improvement said that the run rate earlier in the year suggested the year-end deficit could have been as high as £2.8bn. However there had been improvements in the run rate during the second half of the year, in part a result of measures such as agency and consultancy controls. Providers also realised £724m of ‘financial improvement opportunities’ between December and March, including £324m of local capital-to-revenue transfers.
Publishing the figures, NHS Improvement said that the run rate earlier in the year suggested the year-end deficit could have been as high as £2.8bn. However there had been improvements in the run rate during the second half of the year, in part a result of measures such as agency and consultancy controls. Providers also realised £724m of ‘financial improvement opportunities’ between December and March, including £324m of local capital-to-revenue transfers.
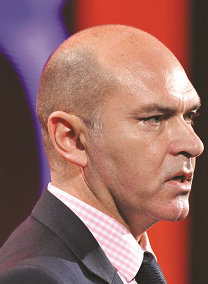
‘When we consider where we were six months ago, NHS providers have done a great job in reducing the planned deficit,’ said Jim Mackey, NHS Improvement chief executive. ‘The key now is for us all to work together to make the necessary improvements in 2016/17 to reduce any variations in the quality of care for patients and to bring the NHS provider sector back into financial balance.’
NHS Improvement’s analysis of the year highlighted significant increases in demand. Accident and emergency department attendances increased by 2.9% compared with the previous year, with a 7.5% increase in March alone compared with the same month in 2014/15.Overall only 91% of patients were seen or admitted with four hours compared with the 95% target.
There was also a 15% increase in the number of patients waiting to start their elective treatment. There was an increase in the median waiting time and providers collectively missed their 18-week referral to treatment target – with just 91% being treated in the required period compared with a target of 92%.
A number of issues were highlighted as having an impact on the year-end position. Providers spent £3.6bn on agency and contract staff compared with a plan of £2.2bn, despite the introduction of agency controls, which NHS Improvement has estimated saved some £300m. Delayed transfers of care cost providers at least £145m, although the regulator said the full costs could be much higher.
Waiting list initiative work to avoid waiting time breaches cost £143m. Despite this, providers paid a total of £751m on fines and readmission penalties, although £253m was reinvested by commissioners to improve operational flows.
To support their financial positions, providers delivered £2.9bn of savings through cost improvement programmes, reducing total year-to-date costs by 3.6%. However this was £316m or 9.8% short of plan and £6m below providers’ forecast at quarter 3.
Paul Briddock, HFMA director of policy, Healthcare Financial Management Association (HFMA), described the financial position as ‘distressing’. ‘The deficit on the provider side of the NHS is incredibly worrying and, given this year-end figure, may now call into question if it is still feasible to balance the department expenditure limit when all the numbers have been calculated.’
King’s Fund director of policy Richard Murray said the figures were unprecedented. 'Overspending on this scale is not down to mismanagement or inefficiency in individual trusts – it shows a health system buckling under huge financial and operational pressures. At the same time, performance against key targets is deteriorating and concerns about quality of care are increasingly widespread.’
Related content
The Institute’s annual costing conference provides the NHS with the latest developments and guidance in NHS costing.
The value masterclass shares examples of organisations and systems that have pursued a value-driven approach and the results they have achieved.