Feature / Portal power
Good cost data is essential to running healthcare services. But it only becomes
really valuable once it is used – ideally by clinicians – to support decision-making or to inform the elimination of waste or the improvement of services.
Alfa D’Amato (right), deputy director of the Activity-Based Funding Taskforce in New South Wales, Australia, understood this early in his career. The point – and his interest – is
Wales, Australia, understood this early in his career. The point – and his interest – is
to transform costing data into clinical insight.
Having trained as an accountant in Italy, Mr D’Amato started his career in Australian healthcare in the middle of the last decade. He soon found himself leading a project to implement ‘episode funding’ for a group of
18 hospitals. He saw the task as improving transparency in his part of the state health system. But it forced him to improve costing data to the point where clinicians would accept it without raising concerns about casemix complexity and without explaining why the data did not apply to them.
This recognition that the clinical workforce is the key audience for cost data has stayed with him throughout his subsequent career.
He joined the Ministry of Health in 2011 to help implement the National Health Reform Agreement, which required all Australian states and territories to introduce a consistent activity-based funding (ABF) methodology.
Initially, Mr D’Amato felt the department did not properly appreciate the opportunities activity-based funding (ABF) could bring. Historically it had relied on population-based funding. But that ‘didn’t lend itself to the level of transparency that enables the system to gain very quickly a level of efficiency that open, shared data can provide,’ says Mr D’Amato.
He now leads the state’s ABF taskforce, which in a few short years has re-engineered patient-level costing across New South Wales and developed an activity-based management (ABM) portal to feed back cost information to clinicians and general managers. A timetable has been agreed to roll out the ABM portal nationwide in Australia.
There are huge parallels with the English health service, whose own casemix funding system (albeit based on healthcare resource groups rather than diagnosis-related groups) predates that in New South Wales. In England too – belatedly some might argue – the NHS is now embarking on a mandatory service-wide implementation of patient-level costing using a common methodology. And NHS Improvement already provides a patient-cost benchmarking tool to voluntary contributors to its patient-cost collection – a forerunner to a future more sophisticated analysis tool.
Back in New South Wales, Mr D’Amato says the programme’s rapid success was down to its structured approach. In year one, the focus was on investment in standardising the IT infrastructure to collect reliable data. In years two and three, he concentrated on maximising data quality so that it could be used for decision making. Now the focus is on using the data and reaping the rewards of the ABM portal. The aim is to extract as much value as possible from the data by making it available to as wide an audience as possible.
The portal allows clinicians and general managers to access the costing information, giving a ‘helicopter view’ of the data at local health district level. IT should mean users can see very quickly where their clinical costing information is an outlier compared with similar hospitals. The data is also submitted to set the ‘national efficient price’ for services in Australia as well as state-wide prices. Mr D’Amato adds that the benchmarking data creates ‘huge competition’ to be seen as the most efficient hospital.
As well as the standard metrics the ABM portal provides, such as average cost and length of stay, it allows analysis of ‘cost buckets’. ‘[It is] so users can see at a particular hospital how the medical staff cost compares to a similar hospital treating similar patients. This allows questions about how to allocate financial resources such as workforce mix between medical, nursing and allied health costs, or to know if it is critical care or theatre costs that need to be examined,’ he explains.
The ABM portal effectively allows users to drill down into the data to identify clinical variation. He says this allows for a much better quality of conversation between managers and clinicians, with clear data and complicating factors such as casemix complexity removed by comparing similar hospitals. He adds that clinicians ‘love’ the portal because they are naturally competitive and relish the opportunity to showcase how efficient their services are.
There are four uses for the ABM portal: benchmarking service costs; identifying and reducing unwarranted clinical variation; reducing the number of high-cost, high frequency patients; and costing patient journeys across sectors and financial years.
Clinicians, managers and finance staff can now ‘benchmark their services across the state in a way they have never been able to before’. Mr D’Amato says two things make this possible. ‘Firstly the data is very transparent, everyone can see everyone else’s data,’ he says ‘and secondly because of the timeframe. Previously it took a couple of years to consolidate all of the data and distribute it, whereas now it is much easier. The most recent benchmarking data was turned around in four weeks from final submission to being available in the data portal’.
Mr D’Amato believes the portal is already a success. ‘We can see the average costs of services are not increasing at the same rate as in the past,’ he says. ‘We’re already bending the curve, which is significant given New South Wales is the biggest jurisdiction in Australia.’ He says the portal has helped identify high-cost patients at risk of multiple hospital admissions, enabling appropriate services to be provided to reduce their overall pathway costs.
It has also allowed the Ministry of Health to demonstrate its efficiency to the state Treasury and other central agencies. The state’s health system is not facing the relentless efficiency and cost improvement requirements of the NHS, but is not immune to the expectation that every dollar will provide the greatest value.
‘Ultimately we want to link our data with patient outcomes data and work towards improving the value of the healthcare we provide, so we can invest in the right areas for the best outcomes.’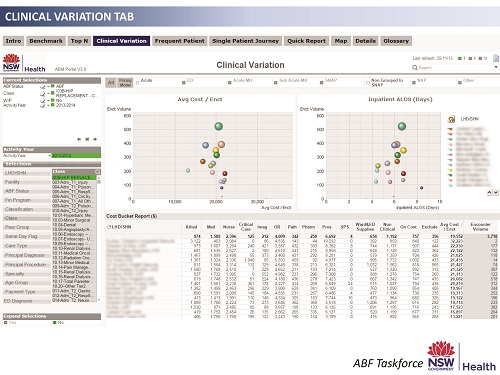
The work is rooted in the academic basis of professors Porter, Kaplan and others – which argue for value-based decision-making in healthcare – but combines it with a typically Australian pragmatism for getting the job done. ‘Unless you are able to demonstrate a direct link with health activity on the ground, it is very difficult to describe what value-based healthcare means to clinicians – is it value for the patient or value for the clinicians?’ says Mr D’Amato.
The mechanics of the data collection that underpin the ABM portal provide some interesting contrasts with infrastructure and practice in the NHS. Mr D’Amato says New South Wales ‘benefits’ from a state-wide, centralised financial ledger system and a similarly centralised approach to patient administration. This has paid dividends in supporting consistent collection of comparable data. ‘The financial and staff time burden of improving data collection are significantly outweighed by the return to patients and improving clinical practice,’ he says.
The ABM portal is also available across all health sectors, including community and mental health. This may seem alien to the NHS based on past payment systems, where such transparency may sometimes have been seen as undermining local negotiations and local pricing arrangements. (However, there are some moves towards open book arrangements in new NHS sustainability and transformation planning footprint areas).
Mr D’Amato says the cross-cutting approach is essential. ‘Often commissioners don’t appreciate the relationships between the services,’ he says. ‘Now they see the relationship between length of stay in acute and mental health services and the provision of sub-acute and community services, for instance.’ Critically, they can see when the overall patient pathway costs less. This is data commissioners have struggled to obtain in the past and, for Mr D’Amato, it is one of his biggest achievements.
As well as seeing benefits across whole patient pathways it has helped relationships between separate parts of the health system. Once the data is transparent and no longer has the potential to cause dispute, the negotiation moves on and costs can be addressed based on the evidence. Mr D’Amato insists there are better conversations to be had between funders and hospitals than arguing about the validity of data. He sees this as a major benefit.
The HFMA’s July NHS financial temperature check survey of finance directors (see page 8) found that only 35% of respondents believe the relationships between organisations in their STP footprint are strong enough to deliver the cross-organisational changes that are required. Given the 2016 contracting round was seen by some as the most challenging in recent memory, how much would newly forming relationships benefit from the kind of data available in an English ABM portal?
Behind the scenes of the portal is a data validation exercise that is crucial to its success. The ABF taskforce provides templates for data collection to ensure consistency, but the audit and assurance of data quality takes place locally, carried out by hospitals’ internal audit teams. Some investment is required, but the pay-off is that data is ready for use almost immediately.
The ability of the ABM portal to benchmark data across the state and, soon, the whole of Australia, is what makes it a game changer, according to Mr D’Amato. Clinicians are having conversations about efficiency, facilitated by finance data and there are genuine improvements to clinical practice and patient outcomes. Funders are having better conversations with their providers.
His message is that this can be done in the UK and the benefits of a goldmine of data for providers and funders will outweigh the short-term pain of setting up data collection systems.
Hear more
Alfa D’Amato will be among speakers to address the HFMA Healthcare Costing for Value Institute’s first international symposium looking at the growing international movement towards value-based healthcare.
The 12 October event will give institute members – including finance leaders and clinicians – a chance to hear in more detail how New South Wales implemented patient-level costing across the state to underpin a cost and activity data portal to support local improvement.
Related content
The Institute’s annual costing conference provides the NHS with the latest developments and guidance in NHS costing.
The value masterclass shares examples of organisations and systems that have pursued a value-driven approach and the results they have achieved.