NHS in numbers: revenue spending
There is also the revenue annually managed expenditure budget (RAME), which is set outside the spending review, is demand-led and relates purely to impairments and provisions that do not need taxes raised to cover spending. Staying within the RDEL is the Department’s key revenue measure and it is set net of income. So it can only exceed the RDEL figure if it has additional income to cover the excess.
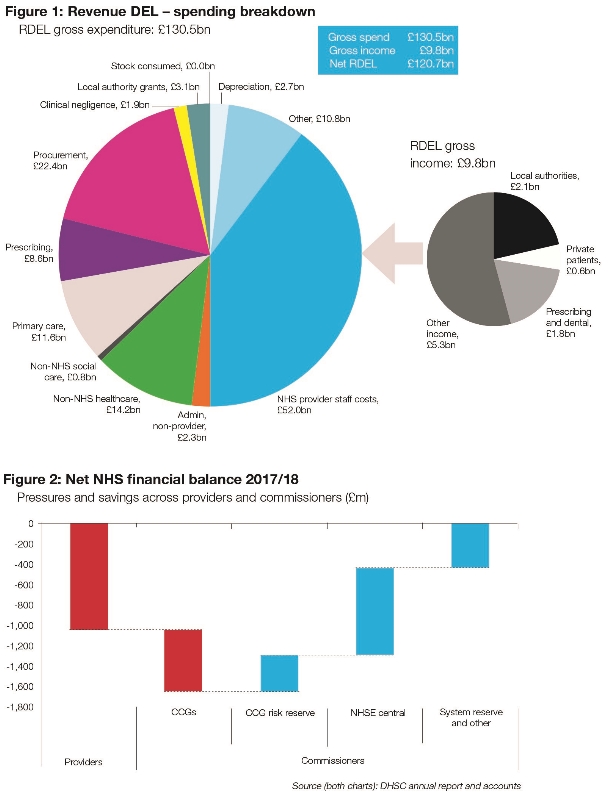
In 2017, the RDEL was £121.3bn. Actual gross spending was £130.5bn, but there was £9.8bn of gross income to be netted off, meaning that actual net spending came in at £120.7bn – an underspend of £692m.
About £76bn of revenue expenditure is within the provider sector and nearly 70% of this relates to staff costs. Provider staff costs (£52bn) in fact make up 40% of gross spending overall, while procurement (£22.4bn), non-NHS healthcare (£14.2bn) and primary care (£11.6bn) are the next biggest items of expenditure.
Of the £121.3bn RDEL budget, £109.7bn was allocated directly to NHS commissioners, with the remainder (£11.6bn) funding arm’s-length bodies and the department’s central budgets.
Providers reported an aggregate deficit of just under £1bn, balanced out by a similar underspend by NHS England (£970m) – meaning that financial balance was broadly delivered for the sector as a whole. Within this, clinical commissioning groups overspent by £600m, reducing to £213m – according to NHS England accounts – after the release of their proportion of a £640m risk reserve.
This risk reserve was set aside in the NHS England allocation to balance out overspends elsewhere in the systems if – as proved to be the case – they were needed. Some £360m of this was set aside by CCGs (based on 0.5% of their allocations).
A further £200m was contributed by NHS England and the final £80m was added to the reserve from other sources during the year. NHS England’s accounts said all three elements were released at the end of the year to offset provider overspends.
However, the CCG element was in fact needed to reduce local commissioner overspends. No risk reserve exists in 2018/19 with the expansion of the provider sustainability fund and the creation of a new commissioner sustainability fund, which will support CCGs in deficit to return to financial balance.In 2017, the RDEL was £121.3bn. Actual gross spending was £130.5bn, but there was £9.8bn of gross income to be netted off, meaning that actual net spending came in at £120.7bn – an underspend of £692m.
About £76bn of revenue expenditure is within the provider sector and nearly 70% of this relates to staff costs. Provider staff costs (£52bn) in fact make up 40% of gross spending overall, while procurement (£22.4bn), non-NHS healthcare (£14.2bn) and primary care (£11.6bn) are the next biggest items of expenditure.
Of the £121.3bn RDEL budget, £109.7bn was allocated directly to NHS commissioners, with the remainder (£11.6bn) funding arm’s-length bodies and the department’s central budgets.
Providers reported an aggregate deficit of just under £1bn, balanced out by a similar underspend by NHS England (£970m) – meaning that financial balance was broadly delivered for the sector as a whole. Within this, clinical commissioning groups overspent by £600m, reducing to £213m – according to NHS England accounts – after the release of their proportion of a £640m risk reserve.
This risk reserve was set aside in the NHS England allocation to balance out overspends elsewhere in the systems if – as proved to be the case – they were needed. Some £360m of this was set aside by CCGs (based on 0.5% of their allocations).
A further £200m was contributed by NHS England and the final £80m was added to the reserve from other sources during the year. NHS England’s accounts said all three elements were released at the end of the year to offset provider overspends.
Related content
The Institute’s annual costing conference provides the NHS with the latest developments and guidance in NHS costing.
The value masterclass shares examples of organisations and systems that have pursued a value-driven approach and the results they have achieved.