Integrated care: one vision, one NHS
The Dorset health and care system is currently organised across nine statutory bodies, six responsible for health and three local authorities. This is set to change over time – on both sides of the health and social care divide – as the Dorset system leadership is committed to the consolidation of entities, not creation of new ones.
Within Dorset, we are fortunate. Not only because of our clean, sandy beaches, but because we have one large countywide NHS commissioner with the scale to host its own in-house ‘commissioning support unit’. And, crucially, we have had continuity of system leadership at all levels in an environment where maintaining trust and effective relationships are so vitally important.
Dorset’s NHS system can also claim a history of relatively strong financial and operational performance. We have good heritage, having previously been strategically led by Sir Ian Carruthers OBE, Ian Tipney and Bill Shields at the helm of the Dorset and Somerset and, more recently, South West strategic health authorities. ‘Do what we said we would do’ has always been our mantra, and we have a solid track record of delivering good services for local patients within the context of also managing upwards with ‘no surprises’.
Dorset has a population of just over 800,000, with more than half living in the urban east Dorset within Bournemouth and Poole. Across our north and west, we have vast areas of rural population. Most of our NHS provision is directly managed by primary, community, secondary and mental health providers within the county.
At an aggregate level, the system works well, but at an organisational level, we have serious sustainability concerns. More than 90% of Poole Hospital’s inpatient activity is currently non-elective. Due to local population demographics, we admit more patients with fractured neck of femur than anywhere else in Britain. We also provide trauma, maternity and paediatric services on behalf of the whole of east Dorset.
Historically, this has limited the organisation’s ability to deliver cash surpluses under the payment by results/foundation trust funding model. This is compounded further as these services attract a disproportionate share of the national risk pooling cost under the Clinical Negligence Scheme for Trusts (CNST).
Sustainability challenge
Each Dorset provider equally has a structural sustainability challenge. All of us recognise that individually we are not sustainable in our current forms. Despite being an all foundation trust health system for many years, both Dorset County Hospital and Poole Hospital have experienced periods ‘under financial investigation’ for reasons of sustainability by the former regulator, Monitor.
However, in autumn 2013, a proposed organisational merger between the Royal Bournemouth (pictured below) and Christchurch Hospitals and Poole Hospital (pictured above) was prohibited by the Competition Commission on the basis of reduced competition not demonstrated to be in the interest of patients. Further, both organisational boards signed a legally binding undertaking not to merge without the explicit agreement of the competition authorities for a further 10 years.
To its credit, Dorset Clinical Commissioning Group responded by launching a full system clinical services review (CSR) in October 2014. Following a structured process of clinical and public engagement, this led to a formal consultation between December 2016 and February 2017 on a significant restructuring of service provision across acute, community, mental health and primary care.
Alongside this, the three acute providers were selected as a national acute care vanguard, with a vision of working towards ‘One NHS in Dorset’. Its aim was to remove organisational barriers to change by enabling joined up clinical and support services, supported by enabling IT systems and infrastructure.
By the time NHS England had called for sustainability and transformation plans to be developed, and created sustainability and transformation partnerships (STPs), collaborative working was already a reality in Dorset.
In committing to our ‘one NHS’ vision, all NHS bodies in Dorset agreed a two-year financial framework for 2017-19. This includes a commitment from the group to deliver its aggregate financial control total commitments, maximising the receipt of national sustainability and transformation funding and related income into our system.
There wasn’t any magic bullet behind our agreement – after all, there was no new money as our commissioner was set to receive almost flat funding. This could only ever sensibly mean ‘flat cash’ contracts for ‘flat activity’, translating into an opening ‘flat workforce’ assumption and significant cost improvement assumptions to offset inflationary cost pressures.
At the same time, we established a monthly governance system to ensure that all parties – individually and collectively – were doing what they said they would do. A formal joint monthly meeting of all chief operating officers and finance directors reports into a system-wide leadership team comprising all chairs and chief executive officers.
Time will tell if this approach continues to work, but the mindset change from 2017 was tangible.
To be completely fair, NHS England and NHS Improvement responded jointly and effectively to our new ways of working. Our journey, alongside other systems, no doubt supported and stretched thinking nationally. This is certainly true in terms of the creation of ‘system control totals’ – Dorset has arguably run ahead of national guidance at times, with support at all times from regulators.
In 2017, the Dorset health and care system was identified as one of eight accountable care system pilots. This would both provide a fast track to improvements set out in Next steps on the five-year forward view and take forward the recommendations of the CSR. And from 2018, the group has been formally recognised by NHS England and NHS Improvement as working towards an integrated care system (ICS).
As part of this, we have already exercised our ability to agree an overall set of net neutral control total offsetting adjustments as part of our 2018/19 operational plans (see table below).
Further in-year offsets of financial over-performance in one organisation against financial under-performance in another are permissible across the ICS, where the overall net impact is neutral.
At this stage, we have not sought to extend our financial risk sharing across health and social care, given the very different financial regimes that underpin the respective sectors. But we will keep this under review.
In 2018, we added a Dorset finance and investment committee to our system governance structure to oversee system-wide investment decisions.
The challenge for the Dorset system remains balancing operational delivery during continued funding restraint, while also creating capacity to achieve an ambitious clinical service redesign across the acute, community and mental health sectors. The east Dorset acute hospital reconfiguration component of the CSR represents a significant change programme, with workforce and operational continuity challenges extending over the next six to seven years.
At the centre of this acute hospital change programme, the Poole and Royal Bournemouth hospitals will specialise as major planned and emergency centres respectively. This brings three key deliverables, alongside sustaining business as usual:
Revisiting the organisational merger that was prohibited in 2013 to create a single clinical leadership to oversee and deliver the commissioner’s model. Both parties are being supported by NHS Improvement to revisit a merger proposal with the Competition and Markets Authority.
Capital investment: £147m has been earmarked for the ICS to enable the reconfiguration of acute services across the two hospital sites concerned. (The CSR’s preferred option was to redevelop Poole as a major planned hospital and the Royal Bournemouth as a major emergency hospital. Detailed planning has been undertaken with outline and full business cases expected to be presented to the Treasury in 2019.)
Reconfiguration of acute services: as already noted, the future for Poole Hospital lies within a merged organisation with the Royal Bournemouth to secure clinical, operational and financial sustainability across the two acute sites. Both sites will be expected to continue to provide existing essential services until completion of the enabling works in 2022/23, with the related clinical and operational efficiencies being delivered from 2023/24.
Financial model
A long-term financial model is being revisited to inform three levels of cash-releasing savings. First, there will be business-as-usual annual cost improvement programme opportunities (before merger assumptions are applied), supplemented by post-merger pre-reconfiguration organisational synergies. On top of this will be clinical reconfiguration efficiency – the total system efficiency element of which is estimated at £19m per year.
More recently and through working together, the Dorset NHS group individually and collectively delivered on its financial ‘control total’ commitments for the year ended 31 March 2018. The system achieved this by broadly delivering on its flat activity, flat cash, flat workforce agreement, supported by new care models outlined in the CSR and sustainability plan (see box).
Several commissioning strategies were adopted to manage demand:
- Referral management – based on peer review and audit
- Commissioning strategies for low-value interventions: reducing activity in areas of limited clinical value
- Encouraging shared decision-making – enabling patients to make informed decisions about their care together with their clinicians
- Redesigning urgent care pathways in primary care to enable a more rapid and effective response to those at risk of an admission
- Proactive case management of patients in the community and risk stratification tools for GPs to enable GPs and community services to focus on at-risk patients and help them manage their condition.
Again, nothing in this list looks like a magic bullet, but by working together to jointly own demand, this has been effective. It has delivered activity trends in most cases better than national averages. Acute referrals from GPs were down 6.4%, creating extra capacity to manage increased urgent care demand, particularly over the winter. Non-elective admissions were up by just 0.6%, which compares with 3.5% nationally, according to NHS Improvement figures. Elective admissions were down 3.1%, due in part to non-elective pressures, but also because of changes in pathways and referrals. Outpatient attendances (first and follow-up appointments) were also down 3.4%. And A&E attendances, in line with the rest of the country, were up 2%.
However, these percentages hide the fact that some providers – including Poole Hospital – have seen a significant increase in the number of patients presenting with more complex and challenging medical conditions by ambulance to A&E. Ambulance conveyances across Dorset were up 6.7% on the previous year.
Despite all bodies having agreed individual and a collective system control total for 2018/19, Poole Hospital needs cash support and has access to this from the Department of Health and Social Care’s uncommitted interim revenue support facility. The trust has already drawn £1.6m repayable cash support during May. This is consistent with the operational and strategic plans agreed with the regulator in 2014, when it exited financial investigation. It will continue until such time that a financially sustainable plan is implemented, and the associated efficiency benefits realised, as part of the CSR.
Given this dependency on external cash funding, organisations such as Poole have limited scope for investment beyond that prioritised as being both urgent and essential for securing ongoing safety and service continuity.
Despite structural financial challenges that relate to the clinical service portfolio, which is not planned to change until 2023, Dorset is performing well across a range of important clinical, operational and value-for-money benchmarks and external assessments (including the Model Hospital, where it benchmarks in the upper quartile, staff survey results and Care Quality Commission ratings).
There are significant pressures, perhaps particularly at the organisational level, but the system is making good progress towards the delivery of more integrated care. There are many challenges ahead, but the first steps appear to be taking us in the right direction.
• Mark Orchard (pictured) is director of finance at Poole Hospital NHS Foundation Trust and immediate past president of the HFMA. He has also worked in other roles across the Dorset system – as finance director at the former primary care trust and at the local NHS England office
Dorset control totals
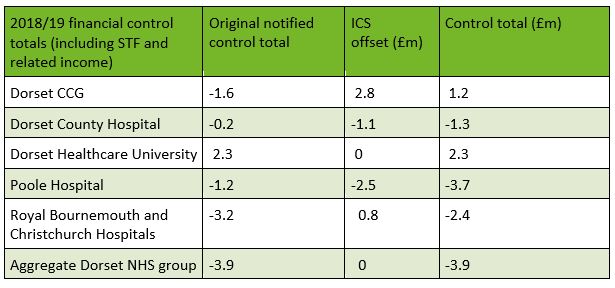 Note: South Western Ambulance Service NHS FT sits outside the control total due to its regional footprint
Note: South Western Ambulance Service NHS FT sits outside the control total due to its regional footprint
Our Dorset
Dorset’s STP plan – Our Dorset – identified three programmes of work to transform healthcare services across the county – prevention at scale; integrated community and primary care services; and one acute network – supported by two enabling workstreams that focused on working differently and maximising use of technology.
The prevention programme aims to help people to stay healthy and avoid getting unwell. This is broken down into a number of strands focused on staying, living and ageing well. Work is ongoing, for example, to support smoking cessation and to expand a health check programme.
As part of the integrated community and primary care services programme, a number of community hubs have been established to provide a focus for a number of services, including rapid same-day access to GP-led urgent care with on-site diagnostics, rehabilitation services and secondary care consultations.
The one acute network strand will deliver the redesigned acute configuration preferred by the clinical services review, which has been through extensive consultation. It is increasingly focused on the renewed merger proposals. The decision to reconfigure Poole and Bournemouth sites into elective and non-elective specialist hospitals has created some retention and recruitment pressures in affected specialties.
As part of enabling works, a single Dorset care record has been established across the county and is expanding its user base.
Related content
The Institute’s annual costing conference provides the NHS with the latest developments and guidance in NHS costing.
The value masterclass shares examples of organisations and systems that have pursued a value-driven approach and the results they have achieved.