Comment / The importance of being earnest about value
Oscar Wilde famously described a cynic – in his play Lady Windermere’s fan – as ‘a man who knows the price of everything and the value of nothing’. Over time, some may feel this label has somehow become applicable to accountants. But 21st century NHS finance staff are increasingly addressing this misconception and are working with clinical colleagues towards a future where they know the value of everything.
This belief is reinforced by the work of the HFMA Healthcare Costing for Value Institute and the NHS Future-Focused Finance (FFF) programme.
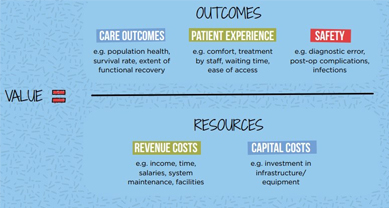
Both these important programmes use a common definition of value – outcomes (including care outcomes, patient experience and safety) divided by the resources used (including both revenue and capital costs).
A common definition of value is essential in a world that is increasingly becoming more complex and system-based. Historically the NHS has relied on individual organisations, run by boards or governing bodies, to deliver care and drive improvement.
However, increasingly organisations are expected to work together in system-based partnerships. This is evidenced by the increasingly important roles of sustainability and transformation partnerships (STPs), integrated care systems (ICSs) and primary care networks (PCNs).
You would like to think that all the different organisations in a system would agree that they had a common goal to deliver good, if not outstanding services. But imagine how difficult future decision making will be if all the different organisations – from commissioners to providers including general practice, local government and the voluntary sector and including regulators – had different views on how to define and measure good.
So, a common definition of value is a big step forward. And that then needs to be followed up with a common decision-making process that puts value into practice – helping systems consistently make value-based decisions.
FFF and the Healthcare Costing for Value Institute are working together to deliver the best possible value decision framework to address this issue. It provides a standardised step-by-step approach that is specifically designed to help systems (or organisations) make value-based decisions. Building on the common definition of value, it uses 12 standard templates/tools that guide people through a structured decision-making process.
Starting with a comprehensive framing of the real decision to be made, it moves onto a methodology for groups to agree what good looks like and how to measure it. There are also templates/tools that help teams manage the project itself and build a value-based evidence log. Ultimately it supports stakeholders to work through different options for a particular decision and ensure the best value choice is identified.
The vital step of ‘actually making a decision, that people own’ is the final part of the best possible value decision framework. The final options are scored by stakeholders using three lenses:
- value, using previously agreed individual weighted value criteria covering the value components of outcomes, experience, safety and resources
- risk, using previously agreed weighted risk criteria, this ensures important issues like operational capacity to deliver the best value option are considered
- strategic factors, scoring previously weighted strategic factors like STP alignment or time to realise benefits.
Finally, the outcome of this three-dimensional scoring approach is presented in a simple graph that shows: the best value option; the lowest risk option; and the options that are strategically aligned.
If one option is best in all three dimensions of scoring then the decision is clear. But usually there is a mixed result, which is then resolved through discussion. This might cover the level of risk that the organisation can accept to implement the otherwise best value decision. Or it might explore the scenario where the best value decision for a particular service is inconsistent with the bigger STP system picture.
This final decision step based on people discussing and owning the decision is key. The best possible value decision framework is simply a tool to aid decision making and it cannot replace the ultimate responsibility of people to make decisions.
We started with Oscar, so let’s finish with him. He also quipped that ‘experience is simply the name given to our mistakes’. Experience tells me with that with the introduction of complex NHS system working and the importance of delivering the new NHS long-term plan, NHS finance staff really need to know the value of everything. This will help people make the right value-based decisions and improve patient care for everybody.
Full details of the best possible value initiative can be found on the FFF website. Contact [email protected] to discuss BPV further.
The value summit, organised by HFMA’s Healthcare Costing for Value Institute and Future-Focused Finance, is on 22 May and features a session on a current BPV project. The day will focus on the importance of clinical and financial collaboration to improve patient care.
Related content
The Institute’s annual costing conference provides the NHS with the latest developments and guidance in NHS costing.
The value masterclass shares examples of organisations and systems that have pursued a value-driven approach and the results they have achieved.