Feature / Focusing on outcomes
Place-based working is key to the success of systems and a recent HFMA roundtable, supported by Newton, explored the key components needed to put partnership working into practice.
Place-based working should be focused on the outcomes it is trying to achieve and ensure it takes into account the views and needs of all partners, especially residents and service users. This was a clear message from a recent HFMA roundtable, supported by Newton, that explored how system partners could put partnership working into practice for the benefit of their local populations.
‘We often seem to start with the task: what we are going to do,’ said roundtable chair Dawn Scrafield, chief finance officer at Mid and South Essex NHS Foundation Trust. ‘What we don’t always talk about are the outcomes that we are trying to achieve.’
Health services can only directly influence a proportion of population health, with wider determinants such as housing and education having a much greater impact. So, if systems are really going to make a difference, they need to have the right partners around the table.
‘We have to bring in the third sector and give them a voice,’ said Alston Owens, assistant director of finance at Torbay and South Devon NHS Foundation Trust. ‘Mental health providers and the third sector all play a massive part, but it is how they can manoeuvre the governance and hierarchical beast of the NHS or local authority – and that can be really difficult.’
He added that this was particularly important given the range of diversity and health inequalities across places and systems. But he said the relationship between the NHS and local authorities was key, with a good working relationship vital. ‘There’s been a wall between the two, but it is starting to come down brick by brick,’ he said. He also raised concerns about the complexity of system working and the language and structures that had been created. The layers of system, place, locality and neighbourhoods were not well understood by the public and this made it difficult to articulate what systems were trying to achieve and at what level.
James Kingsland, former GP and university professor and now an independent healthcare consultant, said a more equitable representation across sectors in the health service was vital given the natural bias in the NHS to focus on secondary care provision.
‘We are still overly focused on making sure we reduce scheduled hospital waiting lists,’ he said, sometimes at the expense of a greater need in the community. With hospital waiting lists a prime performance indicator for the NHS, he said a disproportionate amount of the NHS’s cash-limited resources were concentrated on this area at the expense of, for example, investment in mental health services and social determinants of health.
If the allocative value of the NHS shifted towards more preventative care based in the community, the NHS may start to produce improved longer term outcomes and efficiency in resource utilisation, potentially saving significant public service money downstream.
‘We need an inter-disciplinary, multi-professional approach to delivering care to the diverse population in the UK with increasingly complex care needs rather than following a traditional medical model,’ said Dr Kingsland. And as a start, this means having voices representing more than just acute healthcare around the decision-making table.
Jonathan Webb, director of finance at West Yorkshire Integrated Care Board, said governance arrangements and structure can help. Integrated working in West Yorkshire did not start with last year’s creation of integrated care boards (ICBs). Place-based working, built on the footprint of the former clinical commissioning groups, had been the norm for a while. ‘Our five place committees do include place accountable officers – employees of the ICB – but not exclusively,’ he said. ‘We also have local authority chief executives and directors of adult social care, but they bring together public health, social care, wider local authority services, Healthwatch and community organisations.’
He said this model gave integrated working the best chance. ‘It is all about relationships and trust,’ he added. ‘But the constructs we have now are the best chance we’ve got to deal with the really challenging wicked issues that we face as a society.’
Richard Mellor, finance director of not-for-profit community healthcare provider Locala Health and Wellbeing, said it was not possible to have absolutely everyone round the table and involved in the main groups. ‘So it’s about how you bring those voices in,’ he said. ‘In the Kirklees place in West Yorkshire, we have representatives from third sector parties. But there is also a group in Kirklees of third sector leaders, which then looks to bring more of that group together and is able to input into the place.’ This enables the system to get more voices in the conversation, supporting any specific representative on the place committee.
Financial obstacles
However, he cited obstacles, in particular with organisations being preoccupied with their own financial positions. He said it was difficult to maintain collective conversations when different organisations were focused on their own financial challenges.
Some rules and organisations’ different financial regimes often worked against integrated working, he said. ‘We spend quite a lot of time talking about how we will achieve something rather than getting on and achieving it.’
In his case, as a social enterprise working with the NHS, this often meant worrying about the VAT treatment of joint working rather than focusing on getting improved outcomes. ‘If we didn’t have to work around or with some of the constraints, some of the things we are trying to achieve would be a lot easier,’ he added.
Ric Whalley, a partner for Newton, underlined the importance of getting the right forums and conversations going at ground level. ‘That is where the magic happens in terms of outcomes,’ he said. ‘That is why place is so exciting, because it gets you closer to that ground level.’
Newton has seen good examples of local teamwork – be it around a neighbourhood team or a primary care network. ‘It doesn’t just happen by getting people together – you need to have the right way of working and support them with the right data so they can focus in the right places,’ he said. ‘That is where you can get the real benefit from the wider perspectives. No individual practitioner will have the holistic understanding, given how fragmented services are. But to do the right thing for people, getting those wider perspectives is really key.’
Katy Nex, development director for health and social care at Social Finance, underlined the importance of focusing on outcomes for sustainable system change. But when you did this at place level, she said, you had to balance both short and longer term outcomes. These might involve benefits for the person through better support and for the system, such as improved productivity. For example, a shorter term benefit might be to reduce unplanned urgent care demand to create capacity for elective activity. This would mean the person spends less unnecessary time in hospital and is seen more quickly, alongside the overarching system benefit this creates as waiting times reduce. But places and systems would need to think through the proxies for longer term outcomes such as improvements to life expectancy, which can be hard to measure in a project timeframe.
Matt Williamson, senior finance business partner at Essex County Council, agreed with the importance of ensuring places were focused on what was trying to be achieved and the right outcomes. He said the better care fund had provided a focal point for a lot of joint working between the NHS and social care. But it was easy for the focus to always be on addressing short-term challenges – such as winter pressures or freeing up NHS capacity.
This often meant decisions were effectively taken by NHS or local government colleagues or dictated by available funding. Wider voices were not necessarily heard in those circumstances. Insufficient finance could sometimes be an obstacle to delivering on agreed goals.
He gave an example of a local success story, where the system reviewed the operation of its five neighbourhood teams. It was agreed this configuration did not align well with population needs and a sixth team was needed. This has been taken forward and the NHS and local government have aligned their structures behind the six teams.
But while it was the right thing to do, Mr Williamson said, it involved more investment rather than savings – difficult in the current financial climate. ‘We want to achieve those longer term outcomes, but we can sometimes be constrained by the here and now,’ he said.
Reframe the argument
Amy Whitaker, chief finance officer at Mid Yorkshire Teaching NHS Trust and finance lead for the Wakefield place in the West Yorkshire system, agreed that systems had to find ways to remove financial obstacles or at least reframe the argument. ‘When I took up the place role, the question was very much how we could remove the barrier of finance and focus on long-term rather than short-term priorities,’ she said. There was an assumption that everyone knew what the issue was.
‘The challenge they gave me was: how can we take beds out of the acute so we’ll have the money to invest in communities?’ she said. ‘But how could we make that work when we know the acute already has a deficit of 60 beds? So, before we can even start removing money from the acute, we’d have to save those 60 beds. And then we’d have to take further beds out before we can even start investing in communities.
‘If we wait for that, we are never going to get anywhere,’ she added. ‘So we can keep saying that or we can turn the conversation.’
Instead, Ms Whitaker encouraged a focus on enabling the acute provider to live within its current capacity and understand what is needed across the system to achieve that. ‘Ultimately that should mean the acute doesn’t suck up all the growth in future years,’ she said. ‘If we can do that, it really gives us a pot to start investing in prevention and the community.’
Everyone knew their part in the jigsaw and the contribution needed to achieve this system goal, she said. ‘It has helped with my messaging in the acute, because we are not asking the organisation to take out beds they can’t exist without day to day. But we know we have to live within our capacity,’ she added. ‘The community contribution is through discharge support. And the local authority has to make sure the infrastructure is there around public health and spot purchasing for example.’
The overarching goal is the same – to enable future investment in community and health promotion. But the messaging has changed and everyone is on the same page in terms of what they are trying to achieve.
Ms Whitaker did raise one concern about place-based arrangements. ‘Our places are set up to align with council boundaries, but our population doesn’t observe council boundaries – they just go to the nearest hospital,’ she said. ‘When we are creating places we need to think more about population behaviour rather than focusing on how our councils are set up.’
Dr Kingsland said there was a danger of spending too much time defining and designing place, rather than focusing on the functional aspects of the need to deliver different services at different scales. He also suggested transformational change – moving services from acute settings to the community, say – would need payment reform or bold steps. The only way to change the current model of outpatient services, he said, would be to close the outpatient department and redeploy the staff into the community.
Dr Kingsland said the NHS was still too focused on protecting organisations, despite the ‘whole basis of place-based care being that we didn’t focus care on institutions’. He called for the NHS to get much more comfortable with the idea of implementing proven models of care delivery rather than inventing their own bespoke approaches. ‘If something is working somewhere else, and the evidence is growing, why isn’t that model spreading?’
Phil Morrison, a business manager at Newton, said pilot services could be scaled up for delivery on a broader basis. ‘Quite often we set up an initial pilot – perhaps based on a passion project of a primary care professional – and we don’t enable them to think about how it scales up,’ he said. ‘I think place has a big role to play in deciding the right pilots to take forward and pulling up the right ideas and identifying that they can be applied more widely to broader populations.’
Sometimes it was important to get a pilot up and running before working out all the detail around financing and who employs the staff, he said. ‘We have done pilots where we just make the finance work initially. And when we know we want to scale it, we’ll get the formal frameworks in place to do that. It can be so empowering for the team to just get started.
‘Finances that cross organisational boundaries can just slow things down. So what can we do without having to sort all that?’ he asked. Commissioning issues were the same. ‘Let’s prove the model works first and then argue about who is actually the lead provider afterwards,’ he added.
Mr Morrison suggested that integrated care systems should provide support to supplement the skillsets of those running pilots – helping to set up pilots well, build business cases, use the right data and show how to scale them. He said finance professionals should help systems to understand which schemes could have the biggest impact at scale (see Finance’s place role).
Ms Nex was interested in how new ideas were tested. ‘You need to have something small enough to test it but big enough to demonstrate its impact,’ she said. ‘In the social investment work we do, there is a critical mass you need to achieve for a particular project to demonstrate its impact in the system and not just be noise.’
In terms of data sharing, Mr Whalley highlighted work in Coventry, where the new One Coventry integrated community team gets notified when potentially complex cases are admitted to hospital. ‘That enables them to start planning what they will need for the discharge, rather than beginning near to the point of discharge.
This ‘pull model’ has made a huge difference. Although it is still being scaled up, where it has been working, it has reduced the medically fit length of stay by 50%.
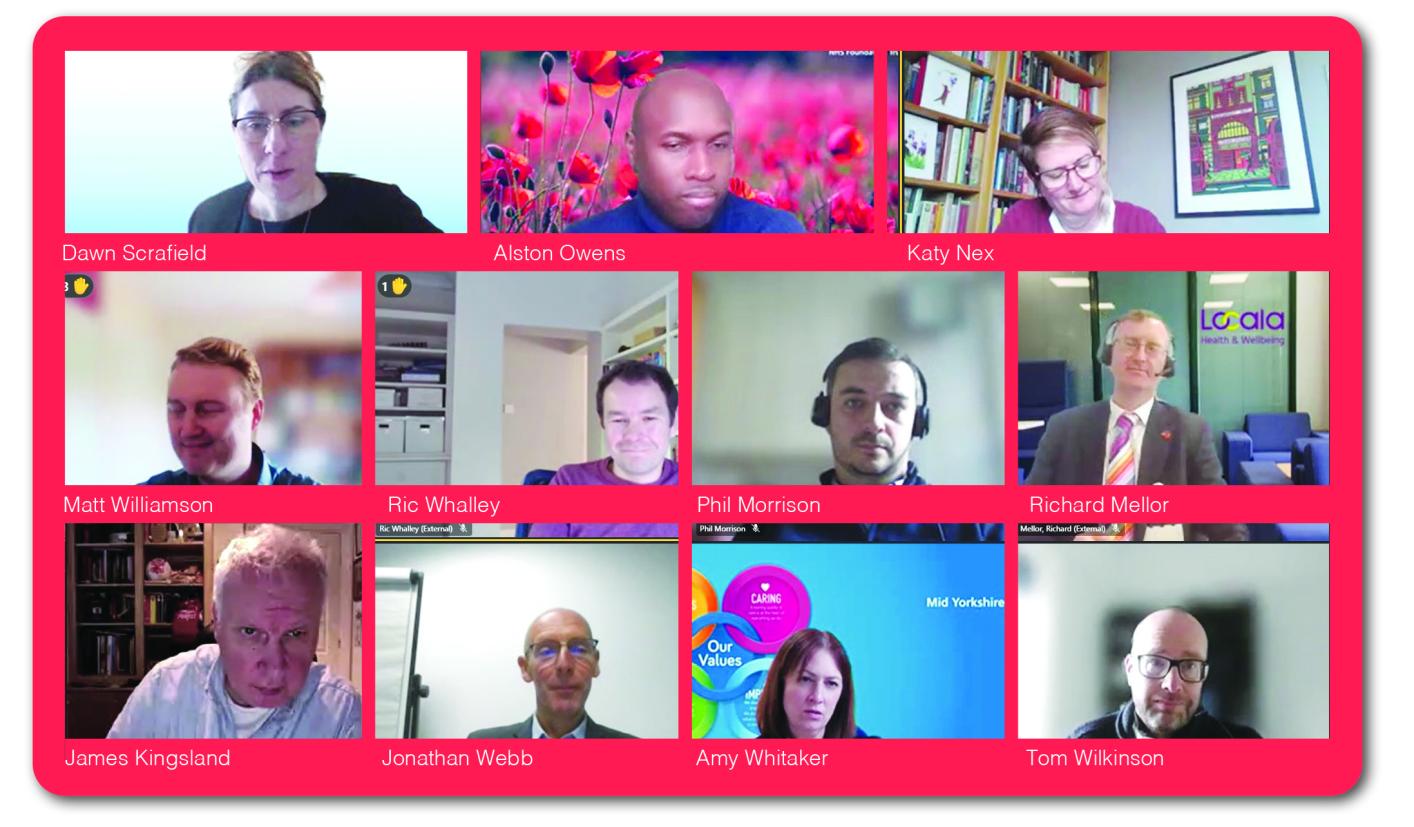
• James Kingsland, University of Central Lancashire; Healthworks.uk
• Richard Mellor, Locala Health and Wellbeing
• Phil Morrison, Newton
• Katy Nex, Social Finance
• Alston Owens, Torbay and South Devon NHS Foundation Trust
• Dawn Scrafield (chair), Mid and South Essex NHS Foundation Trust
• Jonathan Webb, West Yorkshire Integrated Care Board
• Ric Whalley, Newton
• Amy Whitaker, Mid Yorkshire Hospitals NHS Foundation Trust
• Tom Wilkinson, Manchester City Council
• Matt Williamson, Essex County Council
Manchester’s edge
Greater Manchester is often seen as an integrated care leader after its health and social care devolution deal in 2015. Despite this arguably longer run at integration and partnership working, Tom Wilkinson, deputy treasurer for Manchester City Council, said not everything was aligned yet, partially due to the new integrated care board and restructuring of clinical commissioning groups.
Across Greater Manchester, effectively the district councils mapped to the former clinical commissioning group footprints and there have been big strides forward in terms of integrating services, with some joint appointments across health and social care.
But nearly 10 years on, there are still plenty of mismatches. ‘In the city council area, we have 11 integrated neighbourhood teams working in partnership with health,’ he said. ‘But there are 12 primary care networks, so it doesn’t quite fit.
‘And there are other anomalies,’ he added. ‘Mental health gets a bit lost somehow. Mental health funding is massively fragmented, with some money in public health, some in adult social care, some in children’s services and some in the acute setting – and there’s now a bit of money in locality budgets. We need to pull some of that together to maximise the impact it has in a coordinated way.’
He said the financial positions faced by individual organisations could be a big distraction – the significant deficit in the health sector tended to attract all the attention. Despite a desire to move to longer term financial planning, the health service was inevitably focused on its short-term position. He also agreed that there was a tendency for systems and places to ‘follow the money’, with systems bidding for what was available rather than prioritising their local targets.
Ms Scrafield agreed that limited funding was a real problem and the funding that is available is too fragmented. ‘The danger is we all end up looking at the here and now and bidding for something we never knew we needed, rather than staying focused on the things that make more sense for our populations,’ she said.
Participants also raised some concerns about the seeming direction of travel towards greater use of pooled budgets at place level. ‘They are not a panacea,’ said Mr Williamson. ‘Just putting the money together doesn’t solve everything.’ He suggested that for Essex, moving to greater pooled budgets would ‘lose a lot of flexibility around meeting areas of need across our bigger footprint, which crosses multiple places and multiple integrated care partnerships’.
West Yorkshire’s Mr Webb agreed. He acknowledged that sometimes money was the obstacle, and a pooled budget could help. ‘But often it is about trust and relationships,’ he said. ‘Or you may be looking at colocation or using the same IT system. Or it is about agreeing a common outcomes framework. It can be those things that make the difference and you don’t need to bundle all the money together in specific pot to do them.’
In summary, Ms Scrafield said that getting the right people involved with partnership discussions was key to place-based working. And this needed to reach beyond the large NHS and local authority partners.
There should also be a focus on balancing long-term goals with the short-term must-dos. There was a real danger that the long-term objectives and improvements in outcomes could get sidelined by a need to meet the demands of the here and now – with short term financial challenges tending to dominate agendas.
However, she said, financial sustainability and population health improvement depended on places working effectively.
• These topics and good practice examples are explored further in Integration at place – a practical toolkit developed by Newton in conjunction with NHS Providers.
The roundtable considered the specific role for finance teams in helping to make a success of place-based working. Dr Kingsland said the NHS should make those responsible for committing resources – including prescribers and referrers – more accountable for those resources. ‘What we’ve done with clinical teams is put them on committees, we’ve put them on boards, but then they go back to their clinical practice and have no accountability for the efficient use of resources,’ he said.
Ms Scrafield acknowledged that some ‘awareness and transparency’ had been lost, particularly post-Covid, on how resources were spent. If systems continued to work as they do now, more resources would get drawn into the acute sector. ‘How can we help our clinical colleagues understand that better, unless we are sharing information that provides some of that insight,’ she said.
There was agreement that finance teams should be more involved in commissioning decisions. Ms Nex said commissioners often wrongly assumed that finance would be an obstacle. In fact, finance teams are supportive, but haven’t been involved in the discussions. ‘It is just that the commissioning team don’t feel they have system permission.’
Ms Scrafield agreed with the presumption that finance will be a problem without actually asking them. ‘There is something about the narrative that has been created rather than the reality,’ she said.
Newton’s Mr Morrison also highlighted finance teams’ data interpretation skill set. They are good at considering the whole picture and asking the right strategic questions, but are often not involved until the end of the process. ‘We need to bring that forward,’ he said.
He also said finance could be well used to assess the cumulative value of a number of schemes that together could enable cash to be released or resources used more efficiently.
This could leave scheme managers to concentrate on delivering operational value, with the finance team better equipped to determine the aggregate value of a number of schemes.
Related content
The Institute’s annual costing conference provides the NHS with the latest developments and guidance in NHS costing.
This conference provided those responsible for financial reporting the opportunity to start to plan for the financial year-end.