Feature / Cost centre of attention
 When Monitor launched its plans to transform costing across the English NHS back in December 2014, it promised a business case to support its planned switch to more granular patient-level cost data. But while that report is still due to be published later this month, the regulator’s new head of its costing initiative believes in many ways the case is already made.
When Monitor launched its plans to transform costing across the English NHS back in December 2014, it promised a business case to support its planned switch to more granular patient-level cost data. But while that report is still due to be published later this month, the regulator’s new head of its costing initiative believes in many ways the case is already made.
Richard Ford (right), became director of costing for NHS Improvement, which brings together Monitor and the Trust Development Authority, at the beginning of February. He is determined to establish a higher profile for costing in general and the regulator’s Costing Transformation Programme (CTP) in particular. But he says that discussion is now around ‘how’ and not ‘if’.
‘The idea that we need to wait for the value for money report to justify a move to a costing approach – that agenda has moved on,’ he says. ‘Patient-level costing is going to happen. We have the backing of our board, Lord Carter, the Five-year forward view and the BDO report [consultancy report that underpinned the CTP]. The case for change has been accepted while we’ve been developing the value-for-money report.’
A value for money paper, Patient-level information and costing systems – case for change, will be published this month, although Mr Ford says it will be less about identifying exactly how much patient-level costing can save in total and more about helping local organisations to make their own cases locally.
‘It is hard to extrapolate an exact cost-benefit from the case studies we have looked at. But it is clear the benefits easily outweigh the direct costs of costing practitioners and systems. It is also clear that the benefits grow exponentially once costing conversations become embedded, when the finance manager starts to put down the cost centre report and picks up a costing report. By year three, providers have typically recouped their costs and by years three to four in some cases they are getting a three-fold or more return on investment.’
The report will describe the journey on which providers need to go and provide a business case template for providers to take to their own boards.
One thing is clear – the value for money report is no longer being seen as the key trigger for a decision to mandate patient-level costing or new costing standards.
‘The goal is 100% submissions and 100% compliance with a common approach,’ says Mr Ford. He is hopeful the majority of providers will opt to adopt, given the strength of the business case, but recognises that mandating the standards is part of the picture. But he sees the timing of any decision to mandate as being more about what would help trusts most.
While the NHS faces unprecedented financial challenges now and over the coming years, the 2016/17 settlement is relatively better than the later years covered by the spending review. Early mandation – rather than being a tool to push laggards – could actually help trusts take the plunge sooner rather than later, the NHS Improvement director suggests.
Costing pedigree
Mr Ford does not come with a specific NHS costing background. This is in keeping with Monitor’s aim not to populate its central costing team by asset stripping the NHS costing function, which will need to retain and build on existing skill and staffing levels to deliver the programme.
However, he moves from Nottingham University Hospitals NHS Trust, which is in the vanguard of trusts to have implemented patient-level costing and is actively using the data to drive improvement. And his business transformation role at the trust sets him up well for the fundamental overhaul being planned for NHS costing.
He says transformation in the NHS has to be based on delivering better value, measured both in terms of quality and cost. If comparison and benchmarking are to flourish in the way the Carter report envisages, cost data has to be reliable. ‘We are the denominator,’ he says. ‘While we are still working to measure and quantify quality, it is even more important we have costs compiled and reported on a consistent basis across all trusts. It is the one constant we can guarantee.’
And he stresses that the objectives of better costing are to improve reporting and decision-making within trusts, to support benchmarking and to inform pricing. The order is important. NHS Improvement and NHS England’s pricing role demands robust costs, but this is not the prime reason for costing to the patient level.
There has been some solid progress in recent years, but it has been slower than many would have wanted – in part a result of the voluntary approach to adopting patient costing. There is now growing impatience at the centre, as well as rising demand at trust level and a shared recognition that the pace needs to pick up.
Lord Carter’s productivity report has put data and sharing information at the heart of the  transformation agenda. His model hospital envisages whole swathes of data and metrics to support improvement activities and assurance. There are new specific cost metrics – the adjusted treatment cost and the cost per weighted activity unit (see ‘Measure by measure’, Healthcare Finance, March 2016, p20) – but in reality good cost data forms the foundation of the approach.
transformation agenda. His model hospital envisages whole swathes of data and metrics to support improvement activities and assurance. There are new specific cost metrics – the adjusted treatment cost and the cost per weighted activity unit (see ‘Measure by measure’, Healthcare Finance, March 2016, p20) – but in reality good cost data forms the foundation of the approach.
The CTP even gets a specific mention, with the report recommending ‘every effort is made to deliver the programme by the 2020 deadline’. Lord Carter has called for all trusts to be using a ‘standard patient-level costing system by April next year and fully integrated and utilised by October 2018’. Mr Ford admits this is ahead of the CTP timetable and presents ‘ambitious challenges’. Discussions are ongoing.
There has been some wider kickback about the use of reference costs to create these new metrics – given that an audit showed there were material errors in 49% of a sample of cost submissions for the 2014/15 reference costs used. But Mr Ford says Carter is clear that the cost metrics and savings opportunities fed back to trusts are to help them ask questions. And he hopes that overall, the new metrics and Carter spotlight will encourage providers to accelerate their adoption of patient costing.
‘Lord Carter wants us to move at pace because everyone agrees that reference costs have their limitations,’ he says. ‘At the moment, reference costs is the only game in town, but there is no doubt patient-level costing is the future. Lord Carter is right to push us and the service and what is particularly helpful is that he is putting the conversation into the right forum and getting clinicians involved.’
Carter also called for a common chart of accounts to be introduced across England in advance of the costing changes.
However, Mr Ford says he has talked to Lord Carter, who is happy that the CTP approach – translating each trust’s general ledger into a consistent format within a cost ledger with the quantums in both fully reconciled – achieves the same goals.
Progress report
So where is the transformation programme up to? The development of completely new and detailed standards is on schedule, with publication (primarily for roadmap partners) this month alongside the value-for-money report. ‘This has been a massive exercise and very much a bottom-up initiative,’ says Mr Ford. ‘The sector has been fully engaged with finance staff building the standards up from scratch to align with how the BDO report advised costing should work.’
There are 25 in total. Among these are two information requirements, nine costing processes, nine costing methodologies and five costing approaches. For example, one of the costing process standards covers allocating overheads. A methodology standard looks at costing within theatres. An approach standard sets out the costing approach within a specific service area – chemotherapy is an example. And the information requirements examine what source data is needed and how it should be treated. But Mr Ford says they are ‘all standards’, will be compiled in a single costing manual style document and form the basis for any future audit and enforcement. The absolute intention is to allow less room for interpretation and less opportunity for trusts to do things their own way – something the service has called for in earlier consultations.
Mr Ford says NHS Improvement is definitely in listening and collaborating mode. ‘Feedback from the sector suggests the revised approach may in fact be too prescriptive now,’ he admits.
For example, there have been issues with the sheer number of resources and activities being dictated by the centre – meaning that patient cost spreadsheets extend to hundreds of thousands of lines. There are question marks over the value of such detailed analysis and the ability of systems to cope. ‘The point is that we are listening and we recognise we need to find a practical happy medium – a good compromise,’ he adds.
Mr Ford suggests this is in keeping with NHS Improvement’s attempt to position itself as a provider of support to trusts and foundation trusts and not just a regulator.
On the systems front, original plans had been to accredit software to give providers the assurance that existing or new systems were fit for purpose. ‘I’ve asked why we can’t go further and create a preferred supplier database,’ says Mr Ford. ‘Then anyone who needs a new system doesn’t need to undertake a separate procurement process.’ This may take longer at the outset than putting an accreditation system in place, but it will save time overall.
If providers and patients are the main beneficiaries of better costing, then NHS Improvement wants to help providers to help themselves. Some of this is about getting the whole service onto the same page in terms of recognising the benefits of better costing. And some of it is about ensuring it has the capability to compile and use better cost data.
‘The HFMA is a key partner in this,’ says Mr Ford. ‘Our planned engagement strategy will target boards, clinicians and finance staff. Trusts not yet bought into patient costing (literally) will have to demonstrate that their boards have discussed the issue. And where trusts have purchased but not developed their costing systems, we need to get these trusts to the point where they can submit meaningful data. The HFMA has well established networks and we are in the process of identifying and working with partners to help deliver our agendas.’
NHS Improvement is talking directly to the royal colleges about why cost data is a tool for clinicians to deliver better value. And it also wants to support costing practitioners to expand their skills, finance managers to develop costing skills and for the whole finance function to place more value on costing in general.
‘Another key deliverable is the need to grow costing talent. We don’t have nearly enough costing practitioners to deliver our ambitions, so we need the finance community to develop costing talent,’ Mr Ford says.
‘The HFMA is developing a programme as part of its institute to help deliver this. The change comes when trusts are using costing reports in discussions with clinicians, not just cost centre reports. We need to get financial managers doing this, which will get them more interested in costing – and change the perception of costing within and outside the profession.’
There are examples of trusts around the country that are already reaping benefits from patient-level costing. But NHS Improvement believes even these organisations can see greater benefits once all organisations are on board and working to a consistent methodology.
The ability to benchmark is a central theme of Lord Carter’s recommendations, with its calls for the development of a ‘model hospital’ matrix of metrics and indicators. NHS Improvement recognises that cost data is fundamental to this approach. Cost data is already being fed back to participants in Monitor’s voluntary patient cost collection. But the vision is for comprehensive, service-wide information to be provided to all trusts – effectively bringing all organisations into a ‘free’ nationwide benchmarking club.
The ultimate step has to be to put this cost data alongside agreed and consistently measured outcome information – giving a real insight on value. That may still be some time off. But getting the cost data right is an important first step.
The new approach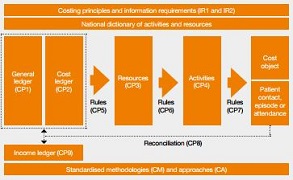
Monitor’s original costing proposals (December 2014) talked about mapping costs from the general ledger into ‘nationally standardised resource categories’ to ensure a common starting point.
In reality there is an intermediate step – creating a cost ledger. This will typically use a combination of cost centre and subjective codes and may involve some disaggregation – for example, breaking down specialist nursing costs into the costs incurred for different types of specialist nursing.
With full reconciliation between the general ledger and standardised resources, this is believed to offer the same benefits as having a common chart of accounts. This has been agreed with the Carter team as achieving the requirements of its recommendation for a standard chart of accounts.
The costs from the cost ledger are then assigned to standard resource categories – covering both direct costs (for example, covering different types of staff in different specialties) and overheads. Resources are then mapped to activities such as ward, outpatient or theatre care. The final stage is to assign the costs of activities to the patients they relate to, either in groups (such as groups of patients receiving general ward care from nurses) or as individuals (a patient receiving radiotherapy or being visited by a district nurse).
Milestone
The Costing Transformation Programme will reach a key milestone this month with the publication of its Case for change report alongside draft acute care costing standards, a Q&A paper, minimum standards for software and resource and activity lists. Mr Ford will also address the HFMA costing conference on 21 April.
Related content
The Institute’s annual costing conference provides the NHS with the latest developments and guidance in NHS costing.
The value masterclass shares examples of organisations and systems that have pursued a value-driven approach and the results they have achieved.