Feature / Blue light approach
Ambulance service providers are making their own rapid response to calls to introduce patient-level costing across the NHS. Steve Brown reports
 The move to patient-level costing in the NHS has largely left the ambulance sector behind. This is perhaps not surprising given that total spending on ambulance services represents only around 2% of total NHS spending in England. There are only 10 dedicated ambulance trusts (plus a combined service trust in the Isle of Wight) across the whole country. And their finance departments do not stretch to dedicated costing teams, with costing oftn being just a small part of an accountant’s responsibilities.
The move to patient-level costing in the NHS has largely left the ambulance sector behind. This is perhaps not surprising given that total spending on ambulance services represents only around 2% of total NHS spending in England. There are only 10 dedicated ambulance trusts (plus a combined service trust in the Isle of Wight) across the whole country. And their finance departments do not stretch to dedicated costing teams, with costing oftn being just a small part of an accountant’s responsibilities.
But NHS Improvement is determined its costing transformation programme will cover all NHS services – opening up the possibility of seeing patient costs across a whole pathway. And that means ambulance service costing is finally getting a bit of attention and support.
The sector may be making something of a standing start in terms of patient-level costing, but the proposed timetable is in fact quite challenging for all parties concerned.
The initial plans to push ambulance trusts through the programme alongside acute trusts were relaxed by a year. But that still leaves ambulance trusts working towards complying with yet-to-be published standards for costing in 2019/20, based on feedback from the ambulance sector, with a fist mandatory cost collection in the summer of 2020.
Bumpy road ahead

These standards are now halfway through their first year of development and NHS Improvement recognises there are
major challenges. ‘There is a lack of experience with patient-level information and costing systems (PLICS),’ says Julia Gray (pictured right), costing standards lead at the oversight body. ‘Until recently none of the ambulance trusts had done patient-level costing before and the majority have not implemented a costing system. There is a clear lack of costing resources and a lack of patient information – the emergency nature of ambulance care means it is simply not captured in many cases.’
To date, the more or less complete focus for costing in ambulance trusts has been the annual reference costs return. This is typically done as a project, with staff returning to their ‘day job’ after submission. A largely top-down process, it provides only average costs. Costs are allocated on the basis of time, but only to produce costs for the average response times for different incidents. It also only covers the 999 work, ignoring trusts’ patient transport and non-emergency 111 work – which together can typically be 25% of a trust’s income.
So moving to more detailed costing for all activities as a year-long process would be a massive step change. NHS Improvement is working with all the ambulance trusts to develop the new standards for the sector – a participative approach that aims to get upfront buy-in for solutions to the key challenges.
One of the most fundamental issues is reflected in the name – patient-level costing. Obviously ambulance trusts’ work is centred around advising, treating and conveying patients. But their operational focus is the incident, not the patient. That is how their activity is counted, how they are paid and how they manage themselves. From a costing perspective, it is also pragmatic. In some incidents, they don’t know the patient they are helping (at least not until later, and sometimes never) – so the cost object would be missing.
Mathew Norman, head of strategic finance at Yorkshire Ambulance Service NHS Trust (YAS), which has recently led the ambulance sector into use of incident-based costing and is one of NHS Improvement’s roadmap partners, says this it is an important distinction.
‘We see huge benefits in more granular costing – but at an incident level rather than at patient-level,’ he says. ‘We get paid per incident and our costs are driven by incidents – for example, we still incur costs if we send a response and there is no patient at the scene.’
While he says the trust does obtain ‘quite a proportion’ of NHS numbers for patients treated or conveyed, this is not comprehensive and some of it requires manual compilation.
NHS Improvement remains committed to being able to see the whole pathway costs for a specific patient. But it recognises the practical difficulties in capturing patient details in all cases. Its solution is to allocate costs to ‘a patient’ not ‘the patient’. So, an incident involving multiple patients only counts as one incident in the currency used to contract for ambulance services (see box overleaf).
But in these cases, trusts would need to record (and make accessible to their costing systems) the number of patients involved. NHS Improvement says this would allow costs to be split among the patients without requiring patient specific information – a good step in the right direction.
NHS Improvement is also aware that ‘time is crucial’ for ambulance services. Their performance management regime has been built principally around response times with associated ambulance quality indicators. ‘Collecting information for costing purposes can never interfere with the processes on the phone or at the scene,’ it says.
Instead, ‘compromise needs to be made to work with the information available,’ says Mrs Gray. Work to date has involved the National Ambulance Information Group to ensure any information collected is used in an appropriate way and, where information is not collected, a work-around can be provided to address this.
Response times
Mr Norman agrees that time is a crucial issue for ambulance services and it is a key driver of its main costs. In some ways, YAS is data rich in this area as it already collects much more detailed time information than the high-level response times set as national targets. For a ‘see, treat and convey’ patient it would collect the times taken for the following:
- Call
- Despatch
- From vehicle start to arrival at scene
- Time at scene
- From scene to destination
- Destination to handover
- Handover to clear
According to Mr Norman, service line management is a strategic priority for YAS, and PLICS is a key component of this. Having a detailed breakdown of how its human and physical assets are used opens up major potential to identify improvement opportunities. ‘We can look at operational information in specific areas, for example, and look at how that impacts variances in average cost, or we could break this down by chief complaint or patient symptoms,’ he says. ‘That enables us to understand the potential benefits of reducing that variation. It might also highlight where to look for examples of good practice.’
The trust is also thinking beyond simple cost analysis. ‘We are starting to look at time spent on scene against patient outcomes,’ he says, adding that specified clinical outcome data is already collected by all ambulance trusts.
‘If we are on scene for just five minutes and then transport the patient to hospital, it may be quicker and cheaper for us, enabling us to get to the next job sooner,’ he says. ‘And it is arguably cheaper for commissioners, bringing down the cost of those journeys. But it may not necessarily be the best thing for the patient or the wider healthcare system.’
Spending more time on the scene could in some circumstances produce a better outcome for the patient and also reduce the pressure elsewhere in the system.
In the detail
Detailed understanding of costs could also help identify the value of different practices and inform redesign across health economies. For example, putting more senior clinicians in vehicles might mean different responses – leaving a patient at home or referring to an alternative service rather than transporting to hospital.
Again, the cost data will enable ambulance trusts to consider the return on investment for the healthcare system when comparing the cost of the senior clinician against the saving in hospital by reduced conveyance. This is of fundamental importance given the current challenges and fits well with the aims of the sustainability and transformation plans.
YAS started introducing its PLICS system in November last year, having selected Bellis-Jones Hill as its provider using the Prodacapo system. Mr Norman says the implementation was planned to last 12 weeks but proved more complex than expected due to the ‘sheer scale of activity and data points in ambulance trusts’.
Yorkshire deals with more than three million incidents a year – up to 900,000 of these are 999 incidents – generating some 4.5 million data points in PLICS. It was a steep learning curve for everyone – the trust, NHS Improvement and the supplier.
Sebastian Kerr, associate director for Bellis-Jones Hill, says the cost model is ‘very different to the one used for acute hospitals and mental health organisations’. Ambulance trusts may only have to allocate costs across four currencies, compared to the thousands of different healthcare resource groups that cover acute activity, but data volumes are still large.
‘In many ways, the data is a lot richer, which makes for a more dynamic understanding of costs because the model can largely be driven by time,’ says Mr Kerr. Or, put another way, high volumes of data but a slightly simpler cost make-up than acute providers.
The trust, supported by its system supplier, is now in an iterative process of refining the process and data. ‘To date, ambulance trusts in general haven’t taken as sophisticated an approach to costing as acutes – mostly because they have not had the staff But YAS has some very capable people, strong data and good informatics support,’ says Mr Kerr. However, while other trusts may have a similar vision, not all have started to put it into action yet.
Mr Norman believes other ambulance trusts should follow YAS’s lead. ‘I can’t overstate the benefits of a PLICS system for ambulance trusts, he says. ‘It increases understanding of the link between performance, resource and finance.’
He is clear it needs commitment from the organisation and support from finance and business intelligence teams – ideally with a dedicated resource internally with previous experience of PLICS. End-users should also be involved at all stages, to avoid the systems being labelled as ‘just another finance system’.
NHS Improvement underlines this message. It has tried to encourage board-level backing for the transformation programme among ambulance trusts and has lobbied for interest with the Association of Ambulance Chief Executives. Now it wants other trusts to follow Yorkshire’s lead and take their own first steps towards patient-level costing.

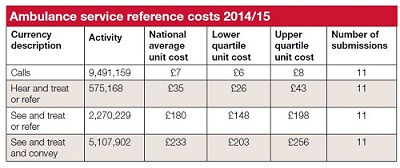
Ambulance service currency
New national currencies for ambulance services were introduced in April 2012 after several years’ development. These form the basis for ambulance trusts’ reference costs submission. While use of the currencies is mandated in tariff guidance, prices are set locally.
There are four activities described by the current currency:
- Urgent and emergency calls answered The unit for payment is per call and all calls to the emergency operations centre are included, including hoax and multiple calls about the same incident. Calls abandoned before being answered are excluded, as are patient transport services requests and NHS 111 calls (both are separately contracted).
- Hear and treat/refer The unit of payment is per incident and covers incidents where the call is resolved by providing advice and an ambulance practitioner does not arrive on the scene. Incidents are included where a vehicle is despatched but called off from attending the scene before arrival. An assumption is that each ‘hear and treat’ involves one patient, so is therefore costed at patient level.
- See and treat/refer The unit for payment is per incident. The patient is treated and discharged from ambulance responsibility on the scene without conveying the patient to a healthcare provider. It also includes incidents where the ambulance professionals are unable to locate a patient or incident.
- See treat and convey The unit of payment is per incident and an incident is counted when at least one patient is conveyed to an alternative healthcare provider. Patient transport services and contracts with non-NHS providers are excluded.
Related content
The Institute’s annual costing conference provides the NHS with the latest developments and guidance in NHS costing.
The value masterclass shares examples of organisations and systems that have pursued a value-driven approach and the results they have achieved.