News / Back in the spotlight
This year’s election marked the high point of discussion of health and social care finances, with all the major parties promising additional funding for the NHS.
Since then it’s been quieter, perhaps due to the focus on talks about Britain’s exit from the European Union and then Parliament’s summer recess. But even without the profile afforded by the election campaign, health service pressure groups, unions and think tanks have still been voicing concern about the future of the NHS.

An early sign that the NHS is set to jump back into the headlines came in a warning from Stephen Hawking about the future of the service. The Brief history of time author, who has lived with motor neurone disease most of his adult life, was concerned about the role of the private sector in the NHS, including the use of agency staff. He claimed the government had failed to undertake ‘proper due diligence’ in respect of the availability of staffing for seven-day services.
He also claimed that there were signs the NHS
was moving to a US-style insurance-based system. This was false, according to health secretary Jeremy Hunt, who added that the proportion of people with private medical insurance had fallen since 2009.
A brief skirmish perhaps, but warnings on the future of the NHS will likely come further to the fore as summer turns to autumn. There will be a short return to Parliament in early September, before party conference season, and then Parliament will be back in full swing from 9 October.
In November or early December, chancellor Philip Hammond will deliver his first autumn Budget. Under a new timetable introduced this year, the Budget timetable has been flipped on its head and the Budget will now be in the autumn, with a financial statement in spring.
In terms of NHS finances, there are a number of things to look out for in the Budget. Will the Conservatives make good on their election pledges to increase NHS funding by £8bn in real terms over the next five years and deliver an increase in real-terms funding per head of population for every year of the Parliament?
The Tories’ commitment to their manifesto has at times been sketchy – as the shift in policy on social care funding showed. And, as with all parties, there’s a talent for sophistry (last Parliament’s controversy over whether health was getting £10bn, £8bn or less over five years is still fresh in many minds). So any announcement on NHS funding will be under the microscope.
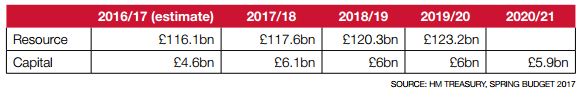
The Institute for Fiscal Studies said the Conservatives’ manifesto pledge suggested an increase in Department of Health spending to £132bn (today’s prices) by 2022/23, assuming all other aspects of Department funding were frozen in real terms. This would amount to an average growth of 1.2% a year between 2016/17 and 2022/23. Current plans – set out in the 2015 spending review – would see an average 0.8% real-terms rise in Department spending between 2017/18 and 2020/21.
On current plans, the IFS said real terms per capita spending is set to fall slightly in 2018/19 and 2019/20, though it will be 3.5% higher than in 2009/10. When the figures are adjusted to take account of the age of the population, however, by 2019/20 age-weighted per-capita spending will be 1.3% lower than 2009/10 levels, it said.
Though any increase in funding will be welcomed, the NHS will have to deal with inflationary pressures, including the pay bill. There was pressure during the election campaign to end the 1% cap on pay rises, with Mr Hunt signalling his sympathy for the case put by the health unions.
Staffing is an issue, generally and in particular specialties and regions, and this is putting additional pressures on pay spending.
An NHS Providers survey, published in July, said that more than 70% of mental health providers expected increased demand this year, but fewer than one in three were confident they had enough staff to deliver the current demand, never mind extending services or creating new ones.
Meanwhile, NHS Digital said that in England NHS bodies advertised more than 86,000 vacancies between January and March this year. Nurse and midwife positions accounted for nearly 40% of these.
The Nursing and Midwifery Council (NMC), which registers nurses and midwives to practise in the UK, said the number of nurses leaving the profession had outstripped those joining for the first time. Although there has been a recent focus on the falling number of nurses from European Union countries registering to work in the UK, the NMC said that the overall downward trend was mainly due to UK nurses and midwives leaving the register.
Capital funding is likely to attract a lot of attention at Budget time. Sustainability and transformation partnerships (STPs) will be hoping for an announcement on capital funding.
In the last spring Budget, in March, Mr Hammond allocated an additional £100m in capital funding to aid A&E department triage and increase provision of on-site GP facilities.
He announced £325m of capital investment over three years for STPs that had the strongest cases for investment – this was allocated in July to 15 areas, including up to £50m for Greater Manchester to concentrate urgent and emergency care across four hub sites.
He promised further STP capital. The Budget document said: ‘In the autumn, a further round of local proposals will be considered, subject to the same rigorous value for money tests.
‘Investment decisions will also consider whether the local NHS area is playing its part in raising proceeds from unused land, to reinvest in the health service.’
During the election campaign, Theresa May committed a re-elected Conservative government to boosting NHS capital funding by £10bn over the course of the Parliament. Backing the recommendations of the Naylor report on NHS property, which was published in March, she said the funds would come from a variety of sources.
The Naylor report said £10bn could be needed and identified the potential for the NHS to release £2.7bn from the sale of surplus property. This figure is adjusted for risk, though the report noted receipts could rise substantially if the NHS takes a more commercial approach to sales – for example, by first obtaining planning permission.
It also said the balance of the required funding could come from the Treasury and private investors. NHS Improvement has explored the potential for private finance to fund new buildings in secondary care and more details may emerge this autumn.
Department of Health budget plans
A&E performance
Operational performance will continue to concern clinicians and managers, as well as the public. The latest figures for A&E waiting times in England show some improvement on the winter months, but it is now two years since the 95% standard was met. In June, 90.7% of patients were admitted, transferred or discharged within four hours. This dropped marginally to 90.3% in July.
In Scotland, 95.5% of patients were seen within four hours in June, but the other devolved nations did less well, though they showed signs of improvement.
In Northern Ireland, 81.2% of patients were seen within the four-hour target in June – an improvement on June 2016, when the standard was met in just over 75% of patients.
In Wales, 84% of patients were seen within four hours in June – 0.7 percentage points higher than June 2016.
It is clear A&E performance throughout the UK is affected, at least in part, by the rising number of attendances and this tide is unlikely to subside in the winter.
Commenting on the NHS England figures,
NHS Providers head of analysis Phillippa Hentsch (pictured) said the service was working at full stretch even during the summer. Despite the efforts to focus on A&E performance, it remained similar to June and July 2016.
‘The lesson here is that there is simply not enough capacity in the system to assure patient safety in the coming winter. We need an immediate decision on whether trusts will be funded to cover the current capacity gap.
‘We estimate that somewhere between £200m and £350m is required – that must be something we can find within an overall health budget of £124bn.’
Urgent action was needed to help the service prepare for winter, she said. Efforts should focus on reducing delayed transfers of care (DTOCs), especially patients waiting for a care package in their own home – in June these patients accounted for 21% of all delayed days.
‘The lack of progress in reducing DTOCs for patients who are ready to move on is particularly worrying, as this leads to longer waits right across the system, including for those who need to be admitted,’ said Ms Hentsch.
‘The increase in DTOCs attributable to social care – especially those waiting for suitable support in their own home – must be addressed.’
The NHS is entering its busiest period with many questions hanging over it, particularly on funding. Some of these will be answered in the autumn and, though additional funding is likely, it could lead to more questions.
Will it be enough or can the NHS safely make up any shortfall?
Related content
The Institute’s annual costing conference provides the NHS with the latest developments and guidance in NHS costing.
The value masterclass shares examples of organisations and systems that have pursued a value-driven approach and the results they have achieved.